Introduction
Although complex dorsal dislocation of the metacarpophalangeal (MCP) joint, also known as Kaplan's lesion, is an uncommon injury, the index finger is most frequently affected.1 They are separated into two categories: simple dislocation, which is reducible without the need for surgery, and complex dislocation, which is irreducible and requiring surgery. 2 Injuries caused by hyperextension of the metacarpophalangeal (MCP) joint frequently result in Kaplan dislocations. The proximal phalanx and the displaced metacarpal head are separated by the volar plate, which is the primary obstruction for closed reduction. Additionally, another three structures—the lumbricals on the radial side, the pre-tendinous band of the palmar fascia, and the flexor tendons on the ulnar side—form a tight constriction noose or button-hole-like phenomenon for the metacarpal head, preventing its reduction. 3
The benefits of open reduction with dorsal approach include adequate view of the volar plate, less danger to volarly displaced neurovascular structures, and adequate exposure for managing osteochondral fractures. But in order to achieve the best reduction, this method necessitates separating the volarplate, which could delay recovery. 4 We are presenting a case of 26-year-old male with a Kaplan lesion of the right index finger post a traumatic event.
Case Report
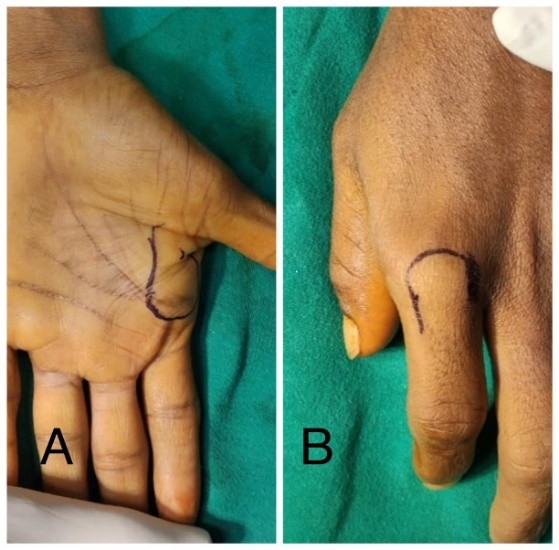
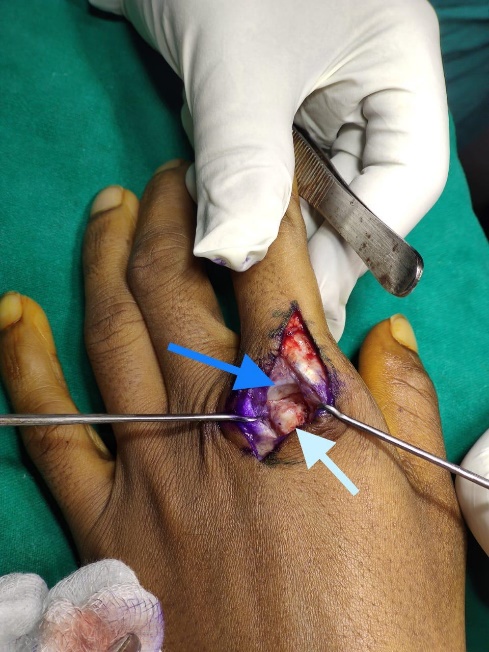
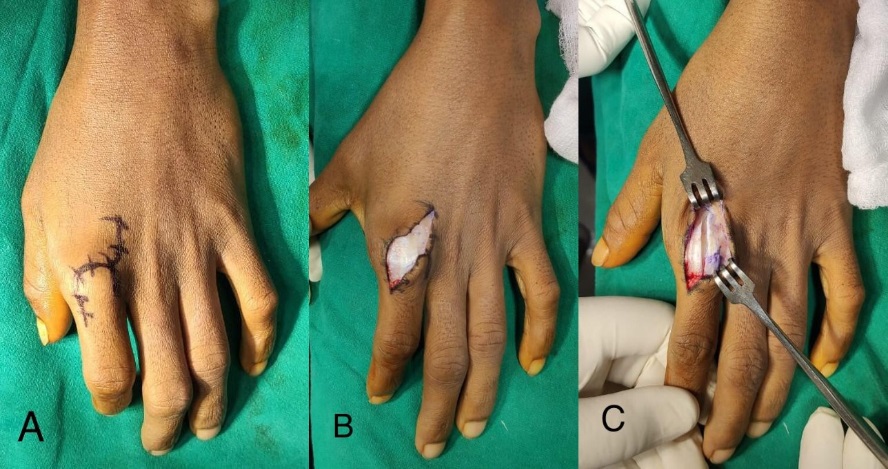
A 26-year-old male presented to our OPD with complaints of pain, swelling and weakness of grip in the right hand for 4 weeks. He gave a history of fall on the right hand while playing kabaddi 4 weeks ago. Immediately after fall he developed pain and swelling in the index finger with an inability to use the hand. He initially took treatment from a local osteopath using native bandages. When he had no relief, he was referred to our department. Clinical findings at presentation included swelling, tenderness on palpation, Metacarpophalyngeal (MCP) joint reduced range of motion and skin dimpling over volar aspect of right index finger (Figure 1). Radiographic views revealed a dorsal dislocation of MCP joint of index finger with a metacarpal head fracture (Figure 2). We decided to attempt a closed reduction initially. The metacarpal head and proximal phalynx were marked prior to reduction (Figure 3). Under digital ring block reduction was attempted, however it was unsuccessful. Then we decided to go ahead with surgical relocation and fixation. A Dorsal curvilinear approach skin incision was taken. Extensor mechanism and joint capsule were incised longitudinally (Figure 4). After further dissection, it was found that the metacarpal head was locked due to volar plate impingement. Metacarpal head osteochondral fracture fragment was found lying at dorsoulnar aspect of MCP joint (Figure 5). The osteochondral fragment was cleared of synovial tissue, reduced and fixed with two K wires. The volar plate was split longitudinally and reduction of MCP joint was done. The reduction was fixed with another K wire (Figure 6). Patient had a good clinical outcome at 6 months post-surgery and returned to all his daily activities.
Post operative protocol included removal of trans-articular K wire at 3 weeks. After 6 weeks, remaining two k-wires were removed and buddy strapping was continued for further 6 weeks. Full activity was restored by the end of 12 weeks.
Figure 4
A: Curvilinear incision marked; B: Curvilinear skin Incision; C: Longitudinal incision over extensor mechanism and joint capsule
Discussion
The radial and ulnar collateral ligaments, which arise from the metacarpal head to the base of the proximal phalanx serve as the main stabilizer of the MCP joint during adduction and abduction. In MCP flexion, these serve as restraints. The volar plate is stabilized by the accessory collateral ligament, which inserts over it and starts anterior to this ligament. In MCP extension, this serves as a static restraint. 5, 6
Radiographs aid in the diagnosis confirmation. A complex fracture dislocation is suggested by a wider joint space and volar plate interpolation. An osteochondral fracture if present can be confirmed on radiograph. 6
Closed reduction attempts should be avoided whenever possible as they increase the risk of osteonecrosis of the metacarpal head or early arthritic degeneration. 7 As soon as our patient arrived, a radiograph was taken, and it showed that the patient had an osteochondral fracture of the metacarpal head and a dorsal dislocation. One unsuccessful attempt was made to close reduction under the digital ring block.
There has been discussion over which of the two surgical intervention approaches—"volar" or "dorsal"—is better. But which one is superior is still a matter of debate. 7 Each approach offers benefits and drawbacks of its own. The dorsal approach was initially described by Farabeuf in 1857, although the Kaplan described the volar approach in 1857. 8 The advantages of the volar approach include direct access to the joint, improved visualization of the tissues, anatomical restoration of the joint, and volar plate repair. On the other hand, the dorsal approach permits the osteochondral fragments of the metacarpal head to be restored, the neurovascular bundle to pass through safely, and the volar plate to be nicely exposed.9 While there is a potential chance of late instability with an unrepaired volar plate, this issue has not been documented for the dorsal approach.6 Additionally, we had a small osteochondral fracture of the metacarpal head, which was easily treated using a dorsal approach.More advanced methods for complex dislocation of the MCP joint, including arthroscopy, lateral approach, and a percutaneous method utilizing a skin hook have been reported.8, 9 Pereira reported in his study that lateral approach can address both volar and dorsal structures with easy accessibility to fixation of osteochondral fragment of metacarpal head. But it risks injury to neurovascular structures.7 During an arthroscopy, the metacarpal head is pulled dorsally and the volar plate is moved palmarly using a probe. Because it only allows for the visualization of the intraarticular structures, arthroscopy is less invasive than open surgery on the structures due to the use of two tiny portals. However, this limitation means that any extraarticular disease or osteochondral fractures cannot be repaired. 10