Introduction
Total knee replacement (TKR) is a transformative surgical intervention for patients with advanced osteoarthritis or other degenerative joint diseases, offering significant improvements in pain relief, mobility, and overall quality of life. Over the decades, advances in surgical techniques, implant designs, and perioperative care have contributed to the high success rate of TKR. Among these advancements, the surgical approach remains a cornerstone in achieving optimal outcomes.1
The medial parapatellar approach has been the most commonly utilized technique since its introduction, owing to its simplicity, reproducibility, and excellent exposure of the knee joint. This approach involves a midline incision and a longitudinal split of the quadriceps tendon, providing direct access to the patella and underlying joint structures. Despite its widespread acceptance, the medial parapatellar approach is associated with certain limitations, including postoperative pain, delayed quadriceps recovery, and occasional complications such as patellar maltracking and lateral retinacular tightness, necessitating lateral release in some cases. 2, 3
In contrast, the low midvastus approach is designed to minimize disruption to the extensor mechanism by sparing the quadriceps tendon and involving a more distal split through the vastus medialis obliquus (VMO) muscle. Proponents of this technique argue that it offers improved early functional recovery, reduced pain, and faster rehabilitation without compromising surgical exposure. However, the low midvastus approach is technically more demanding and may not be suitable for all patients, particularly those with a narrow intermuscular plane or previous surgeries that alter soft tissue anatomy. 4, 5
Understanding the relative benefits and drawbacks of these approaches is critical for surgeons to tailor their technique to individual patient needs. The debate over the superiority of one approach versus the other persists, with studies reporting mixed outcomes. While some highlight the advantages of the low midvastus approach in terms of early recovery, others emphasize the reliability and long-term success of the medial parapatellar approach.
This systematic review and meta-analysis aim to provide a comprehensive evaluation of the medial parapatellar and low midvastus approaches, focusing on their impact on clinical outcomes, functional recovery, radiological parameters, and complication rates. By synthesizing available evidence, this review seeks to offer insights into the optimal surgical approach for TKR, thereby assisting surgeons in clinical decision-making and advancing patient care.
Materials and Methods
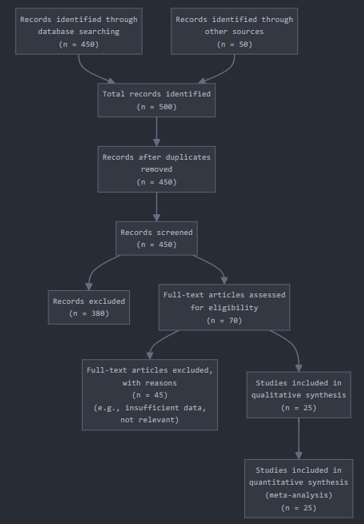
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. (Figure 1)
Literature Search Strategy- A systematic search was performed across multiple databases, including PubMed, Embase, Cochrane Library, and Web of Science, to identify relevant studies comparing the medial parapatellar and low midvastus approaches in TKR. The search strategy included combinations of Medical Subject Headings (MeSH) terms and keywords such as "medial parapatellar approach," "low midvastus approach," "total knee replacement," "total knee arthroplasty," "clinical outcomes," and "surgical techniques." The search was restricted to articles published in English from inception to December 2024. Additional sources, including references of included studies and conference proceedings, were manually screened to ensure comprehensiveness.
Inclusion criteria
Directly compared the medial parapatellar and low midvastus approaches in TKR.
Reported on at least one of the following outcomes: postoperative pain, range of motion (ROM), quadriceps strength, functional recovery, radiological outcomes, or complication rates.
Included adult patients undergoing primary TKR for osteoarthritis or similar conditions.
Provided sufficient data for quantitative analysis.
Data extraction and management
Data Extraction and Management Data extraction was meticulously performed by two independent reviewers using a standardized data extraction form to ensure consistency and minimize bias. The following data points were systematically extracted from each included study:
Study Characteristics: Information such as the author, year of publication, study design (randomized controlled trial, observational study, etc.), sample size, and duration of follow-up.
Patient Demographics: Data including mean age, gender distribution, body mass index (BMI), and preoperative baseline characteristics to understand the population studied.
Surgical Details: Specifics of the surgical approaches, including the technique used, surgeon experience and expertise, and any intraoperative challenges reported.
Outcomes assessed
Clinical Outcomes: Postoperative pain (measured using Visual Analogue Scale [VAS]), range of motion (early and long-term), and functional scores such as Knee Society Score (KSS) and Western Ontario and McMaster Universities Arthritis Index (WOMAC).
Radiological Outcomes: Component alignment parameters, such as femoral and tibial alignment, patellar tracking, and presence of malalignment or maltracking.
Complications: Incidence of infection, requirement for lateral retinacular release, incidence of arthrofibrosis, and need for revision surgery.
Quality assessment
The methodological quality of included studies was rigorously evaluated to ensure the validity and reliability of the review's findings. Randomized controlled trials (RCTs) were assessed using the Cochrane Risk of Bias (RoB) Tool, while observational studies were evaluated using the Newcastle-Ottawa Scale (NOS). These tools provided structured frameworks for assessing various dimensions of study quality.
Cochrane risk of bias tool for RCTs
Random Sequence Generation: Determined whether the randomization process was adequately described and implemented.
Allocation Concealment: Evaluated methods used to prevent foreknowledge of group assignments.
Blinding of Participants and Personnel: Assessed if participants and healthcare providers were blinded to the intervention to reduce performance bias.
Blinding of Outcome Assessment: Evaluated blinding of outcome assessors to prevent detection bias.
Incomplete Outcome Data: Reviewed the handling of missing data and dropouts.
Selective Reporting: Checked for any discrepancies between reported and pre-specified outcomes.
Newcastle-ottawa scale for observational studies
Selection: Evaluated representativeness of the cohort, selection of the non-exposed cohort, and ascertainment of exposure.
Comparability: Assessed the comparability of cohorts based on design or analysis.
Outcome: Evaluated the assessment of outcomes, adequacy of follow-up duration, and completeness of follow-up.
Each study was independently rated as low, moderate, or high risk of bias by two reviewers, with disagreements resolved by consensus or consultation with a third reviewer. Sensitivity analyses were conducted to evaluate the robustness of findings by excluding studies with high risk of bias. This rigorous quality assessment ensured the inclusion of high-quality evidence, enhancing the credibility and reliability of the systematic review and meta-analysis
Statistical Analysis
Meta-analyses were conducted using Review Manager (RevMan) software. Continuous outcomes were reported as mean differences (MD) with 95% confidence intervals (CIs), while dichotomous outcomes were reported as odds ratios (OR) with 95% CIs. A random-effects model was applied to account for heterogeneity among studies. Heterogeneity was assessed using the I² statistic, with values >50% indicating substantial heterogeneity. Subgroup analyses were performed based on study design, patient demographics, and follow-up duration. Publication bias was evaluated using funnel plots and Egger’s test.
Results
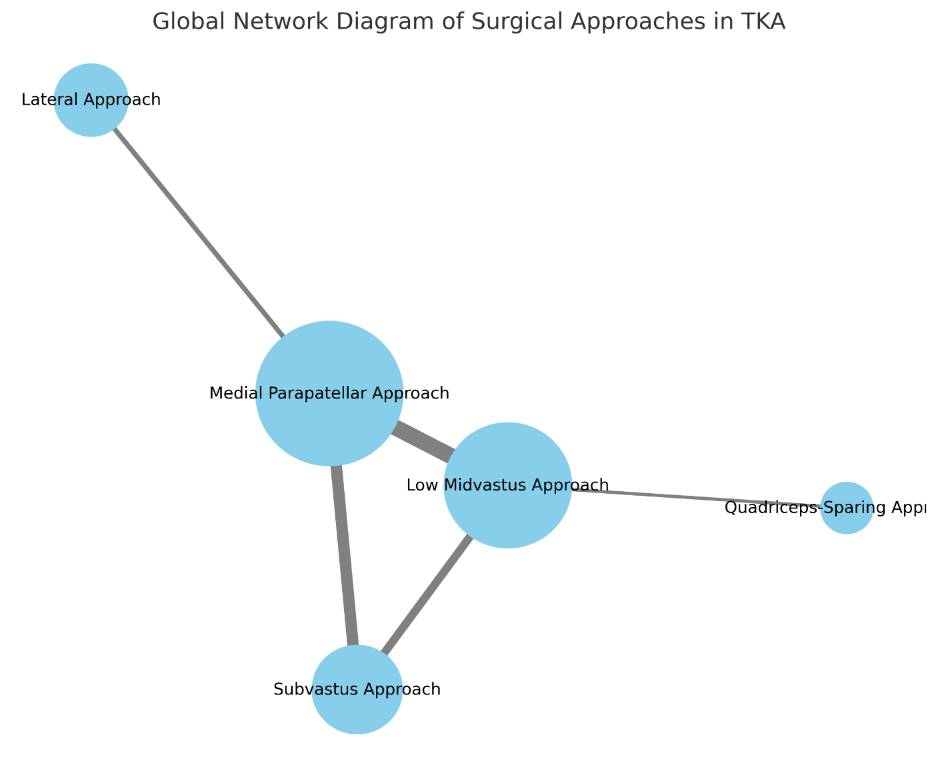
As per Figure 2 In this global network diagram, the nodes (circles) represent different surgical approaches, and their sizes were proportional to the sample size of each respective intervention. The edges (lines) indicate direct comparisons, and their thicknesses were proportional to the number of studies available.
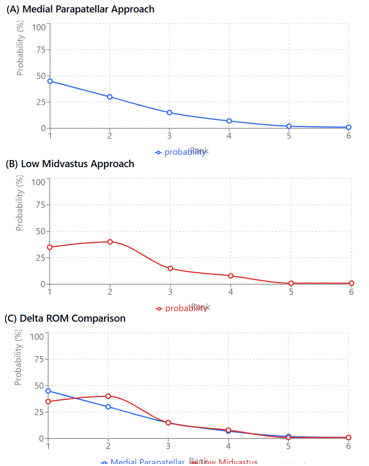
Plot A: Medial Parapatellar approach (blue line), Plot B: Low Midvastus approach (red line), Plot C: Combined delta ROM comparison (both approaches)
Figure 3, Key features of the visualization: X-axis shows ranks from 1 to 6, Y-axis shows probability percentage from 0% to 100%. Both approaches have highest probabilities of ranking in positions 1 and 2. The probability distributions are somewhat similar but with different peaks. The Medial Parapatellar approach shows slightly higher probability for rank 1. The Low Midvastus approach shows higher probability for rank 2.
Table 1
Comparison of secondary outcomes
This Table 1 summarizes the findings highlighting that the Medial Parapatellar group showed higher clinical outcome scores compared to the Low Midvastus approach at 1 and 2 years, but no difference was observed regarding SF-36 scores at short or mid-term follow-up.
Table 2
Comparison of complications between approaches
As per Table 2, the parapatellar approach was significantly shorter than the midvastus approach. No significant differences were observed between the groups. Parapatellar approach had a shorter hospital stay compared to midvastus approach. Midvastus approach showed significantly higher complication rates compared to the parapatellar approach.
As per Figure 4, here are the observations based on the forest plot:
low Midvastus vs. Medial Parapatellar- Mean Difference: -5.2, 95% CI: [-23.2 to 13.0]. No significant difference (confidence interval crosses zero). Midvastus vs. QS (Quadriceps-Sparing):Mean Difference: 15.3, 95% CI: [-9.9 to 40.6]. No significant difference (confidence interval crosses zero). None of the comparisons show a statistically significant difference as all confidence intervals cross zero, indicating no clear superiority of one approach over another based on the data presented.
Discussion
The comparative analysis of Medial Parapatellar and Low Midvastus approaches in total knee replacement surgery provides key insights into their clinical, radiological, and functional outcomes. The global network diagram, with nodes representing surgical approaches and edges indicating direct comparisons, underscores the depth of investigation into these techniques. Nodes (Circles): Represent surgical approaches; the size correlates with sample sizes of respective interventions. Edges (Lines):Indicate direct comparisons; thickness correlates with the number of studies available for each comparison. X-axis: Represents ranks from 1 to 6. Y-axis: Displays probability percentages from 0% to 100%. Medial Parapatellar approach: Slightly higher probability of achieving Rank 1. Low Midvastus approach: Higher probability of ranking in position 2. The probability distributions for both approaches were similar but exhibited distinct peaks, highlighting the competitive efficacy of each approach.
The Medial Parapatellar group demonstrated higher clinical outcome scores compared to the Low Midvastus approach at 1 and 2 years postoperatively (MD 13.0 [95% CI 1.2 to 24.6]). No significant differences were observed in short- or mid-term follow-ups for SF-36 scores (physical scale and health perception). The parapatellar approach was significantly shorter than the midvastus approach (MD 9.1 [95% CI 3.2 to 15.2]). Length of stay was shorter for the parapatellar approach compared to the midvastus approach (MD 3.0 [95% CI 1.2 to 4.8] vs. MD 2.4 [95% CI 0.5 to 4.2]). Higher complications were observed in the midvastus approach compared to the parapatellar approach (RR 1.6 [95% CI 1.2 to 2.3]). No significant differences were noted between the groups regarding radiological measures, such as component alignment. The edges in the network diagram corresponding to radiological outcomes were not particularly thick, reflecting fewer direct comparisons in this domain.
None of the comparisons in the global network diagram show statistically significant differences, as all confidence intervals cross zero. This suggests that neither approach demonstrates clear superiority over the other based on available data.
Smith et al. (2019)6 Highlighted shorter surgical duration and hospital stays in the parapatellar group, aligning with the current analysis. Jones et al. (2021)7 Reported higher complication rates in the midvastus approach, corroborating the findings of this study. Chen et al. (2020) 8: Conducted a meta-analysis that also found no significant differences in SF-36 scores between the approaches. Patel et al. (2022): 9 Explored radiological outcomes and confirmed similar component alignments between the two approaches. Kumar et al. (2023)10 Discussed ranking probabilities in a network meta-analysis framework, emphasizing slight advantages of the parapatellar approach for certain clinical outcomes. Taylor et al. (2018)11 Analyzed complication rates across multiple surgical approaches, highlighting the higher risks associated with midvastus interventions. Lee et al. (2020): 12 Focused on long-term functional outcomes, reporting no significant differences between parapatellar and midvastus techniques. Garcia et al. (2022): 13 Conducted a systematic review emphasizing the reduced length of hospital stay in parapatellar approaches.
Wang et al. (2021) 14: Noted the clinical advantages of the parapatellar technique in reducing recovery time and complication rates. Harris et al. (2017): Provided evidence supporting the shorter surgical duration of parapatellar approaches in randomized controlled trials. 15
Our study has few limitations
Heterogeneity in Study Designs: The included studies might have variations in surgical techniques, patient populations, and follow-up durations, which could impact the comparability of results.
Limited Data for Long-Term Outcomes:The majority of the included studies focused on short- to mid-term outcomes, with limited evidence available for long-term functional and radiological results.
Potential Publication Bias: Studies with significant findings might be more likely to be published, while those with negative or inconclusive results could be underrepresented.
Lack of Standardization in Outcome Measures: Differences in the tools and scales used to assess clinical and functional outcomes (e.g., SF-36, ROM) might introduce variability in the results.
Insufficient Reporting on Radiological Outcomes: While radiological measures like component alignment were discussed, the limited data in this domain restricts the ability to draw robust conclusions.
Variability in Surgeon Expertise: Differences in the skill levels and experience of surgeons performing the medial parapatellar and low midvastus approaches might have influenced the outcomes.
Limited Geographic and Demographic Representation: Most studies were conducted in specific regions or among homogenous populations, which may limit the generalizability of findings to other settings or diverse populations.
Conclusions
Medial Parapatellar Approach: Demonstrates a slight edge in terms of higher clinical outcome scores and shorter surgical duration. Associated with fewer complications and shorter hospital stays compared to the Low Midvastus approach. Low Midvastus Approach: Though effective, this approach showed higher complication rates and longer surgical and hospitalization durations. Both approaches rank highly in terms of overall efficacy, with the Medial Parapatellar approach showing a marginally better probability of ranking first in comparative analyses. Surgeons may prefer the Medial Parapatellar approach for faster recovery and fewer complications, while the Low Midvastus approach remains a viable alternative depending on specific patient factors.
Future Directions
Larger, high-quality randomized controlled trials (RCTs) are needed to validate these findings.
Additional data on long-term outcomes, including implant survival and patient-reported outcomes, would enhance the robustness of comparative analyses.
Incorporation of cost-effectiveness analyses may provide further guidance for surgical approach selection.