Introduction
Synovial chondromatosis is a monarticular svnovial proliferative disease in which cartilaginous or osteocartilaginous metaplasia occurs within the synovial membrane of joints, bursae or tendon sheaths.1
The disease nas been classilied into three phases
Early: with svnovial chondrometaplasia but no loose bodies:
Transitional: with active svynovial disease and loose bodies and
Late: With loose bodies but no synovial disease.
Cartilaginous metaplasia from joint, tendo, or bursal synovial lining differentiates this entity from loose bodies arising from degenerative arthritis, osteochondritis dissecans. and osteochondral fractures. 2
Carlos Renato Ticianelli Terazaki MDs, 3 Residents, Unit of Radiology and Imaging Diagnosis, Hospital São Vicente - Funef, Curitiba, PR, Brazil reported that In spite of being less common than in other joints of the body, synovial osteochondromatosis may be found in the shoulder at the level of the joint recesses (including the tendon sheath of the biceps long head) and in the subacromial-deltoid bursa. The diagnosis may be achieved only on the basis of typical imaging findings which, depending on the stage of the disease, may correspond to synovial membrane proliferation, presence of cartilaginous nodules (chondromas) and calcified or ossified nodules (osteochondromas).
Balakrishnan M. Acharya a, Pramod Devkota 4 reported that Synovial chondromatosis of shoulder have been rarely reported in the literature and most reported are case series only. The etiology of synovial chondromatosis is not known but it is classified as primary or secondary and the secondary is due to trauma, rheumatic arthritis, tubercular arthritis, osteochondritis dissecans. Also may present local pain and tenderness with swelling on the joint. X-ray may not show clearly on not calcified swellings and magnetic resonance imaging (MRI) scan is needed for clear findings.
Case Presentation
History
A 54 Year Hindu male, moderately built and nourished, presented to the orthopaedic OPD with complains of pain and swelling in left shoulder since one year which was insidous in onset, gradually progressive in nature and not relieved by medications. Patient also complained of clicking noise during shoulder movements which was insidous in onset and gradually progressive in nature. The patient had no history of Diabetes Mellitus / Hypertension / Asthma / Tuberculosis / Cardiac Condition / Previous Surgery / Shoulder Injury. The patient had no specific family history of any tumour or shoulder pain. The patient had visited multiple doctors and got multiple X-rays done and taken courses of NSAIDs but had found no relief.
Examination
On clinical examination, Supraspinatus Neer impingement test was moderately positive, tests for other rotator cuff muscles were normal. Patient had decreased ROM in all planes and painful movements were noted.
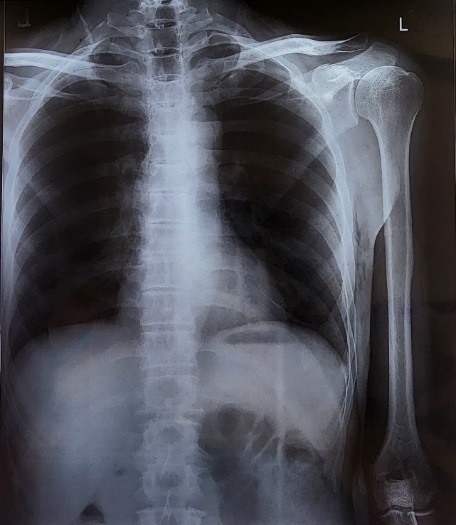
Investigations
After initial evaluation with an X-ray, an MRI was done which revealed Large lobulated soft tissue thickening in the anterior joint capsule extending from subacromial bursa through subcoracoid bursa and from anterior joint capsule to lower joint capsule with maximum thickness in anterior part of 18mm with minimal reactive effusion s/o synovial chondromatosis. There was also increased signal intensity and thickening of the supraspinatus tendon s/o tendinosis.
All routine investigations were done, CBC, PTINR, RBS, RFT, LFT, S.ELECTROLYTES, HIV, HBSAG, HCV and were within normal limits.
Pre-Anaesthetic Checkup was done and patient was posted for surgery. Patient was given an anxiolytic preop (Tab Alprazolam 0.25 mg). Preoperative antibiotic was given (Inj Ceftriaxone 1gm IV). (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6)
Figure 2
MRI Image STIR Long - MRI image of coronal section of left shoulder joint STIR long image preoperatively
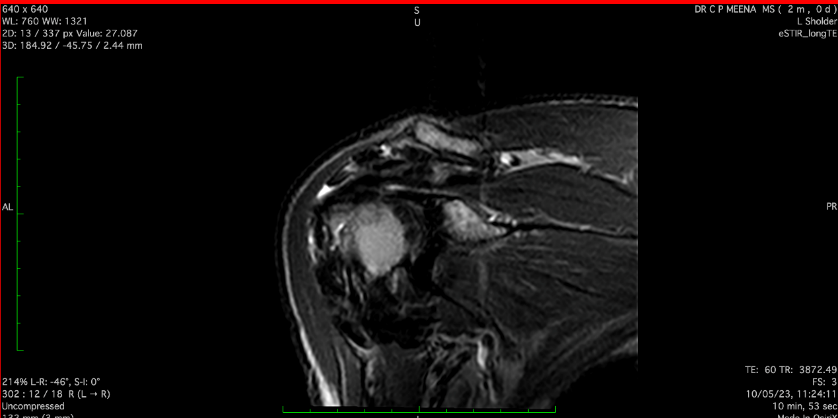
Figure 3
MRI Image T1W - MRI image of coronal section of left shoulder jointT1W image preoperatively

Figure 4
MRIimage SPAIR - MRI image of axial section of left shoulder Joint SPAIR image preoperatively
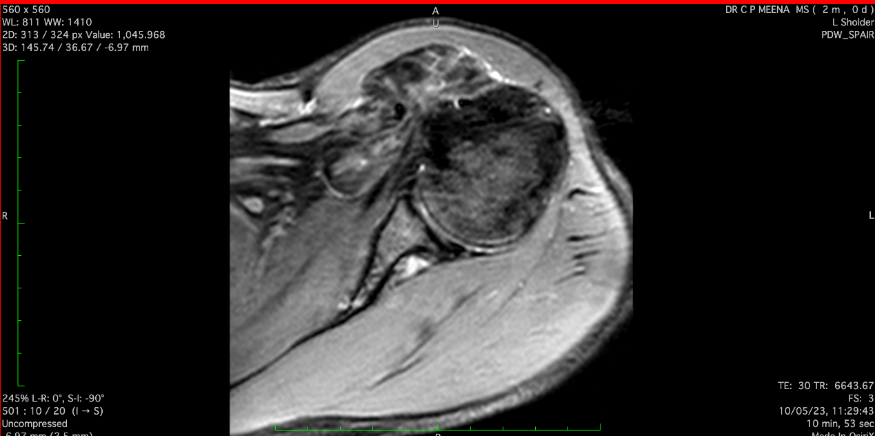
Figure 5
MRIimage eSPAIR - MRI image of axial section of left shoulder joint extended SPAIR Image preoperatively
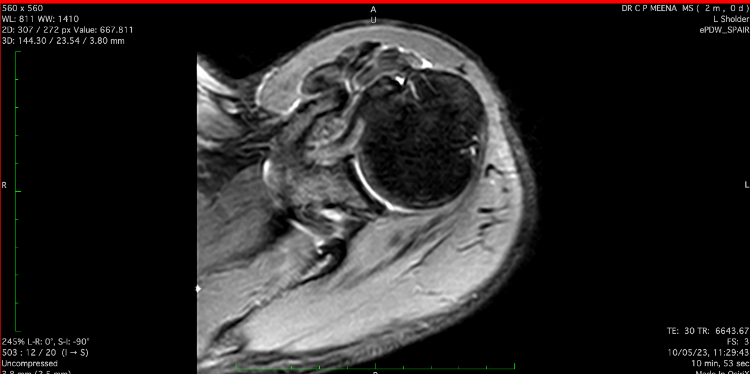
Figure 6
MRI image localizer- MRI image of coronal section of left shoulder joint localizer image preoperatively.
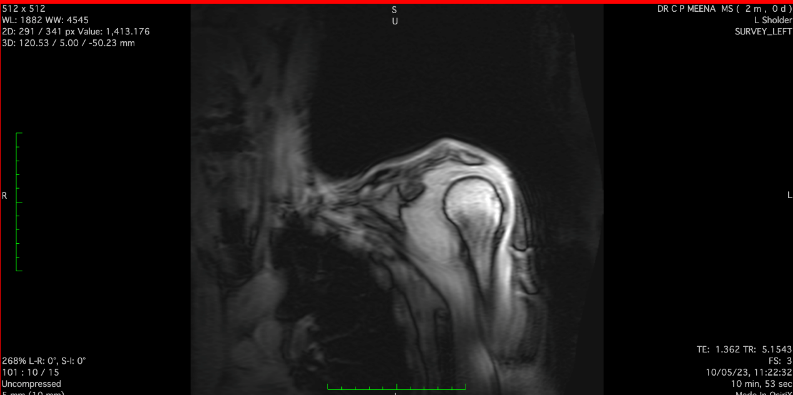
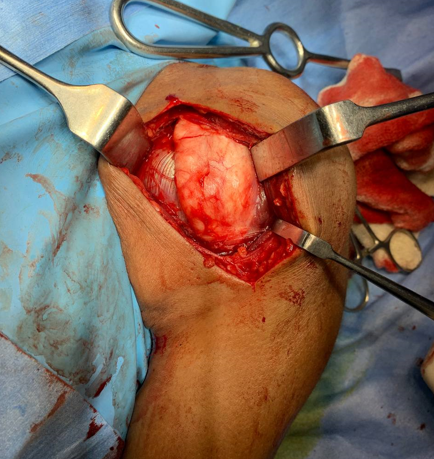
Figure 8
Dissection of Planes - Operative Image of Dissection of Planes, localization of Cephalic VeinIntraoperatively of Patient
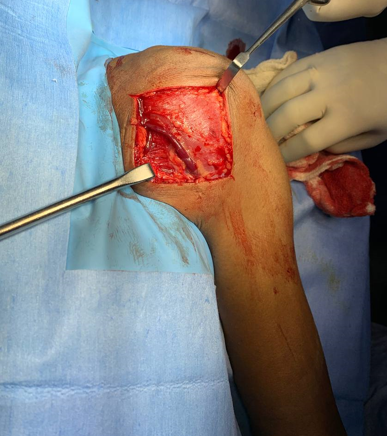
Surgery
After optimization of the patient and written informed consent, patient was taken to the OT, a deltopectoral approach was used. Cephalic vein was identified and preserved and planes were dissected. Partial synovectomy was done and wound was thoroughly washed and closed in lavers. Postop period was uneventful and patient was discharged on POD 2 after clean and sterile dressing. Patient was called to OPD and sutures removed on POD 12. Wound was healthy and patient recovered uneventfully. (Figure 7, Figure 8, Figure 9, Figure 10, Figure 11)
Histopathology report received on POD 14 stated: On gross examination: approximately 8x5x3cm grayish white, irregular soft tissue specimen.
Discussion
Synovial chondromatosis is a synovial lesion seen generally in adults with a male predominance. It occurs most commonly in the knee, unsually also occuring at the hand, wrist, elbow and shoulder.5 It can lead to mechanical symptoms, decreased range of motion and effusion. Histopath shows nodules of moderately cellular hyaline cartilage. 6 D/D can include Myositis Ossificans, Synovial Chondrosarcoma and Synoval Sarcoma. Treatment is usually observation if asymptomatic.7 It symptomatic, then arthroscopic or open synovectomy can be done, arthroscopy increases chances of recurrence.
Toru Ichisek reported that In the present case RSA for primary SO, complicated by prominent arthropathic changes and a massive rotator cuff tear, was associated with a good postoperative course.8 SO was thought to have been most likely implicated in the underlying pathophysiology of this case. 9, 10
The take home message for this case report is that not all patients with chronic shoulder pain and mechanical issues may have benign disorders and should always be worked up lest we miss an important diagnosis for lack of knowledge on the healthcare provider’s side.
Conclusion
Although shoulder is a rare site, synovial chondromatosis may still occur at this joint especially in the joint recesses. This disease can only be diagnosed by imaging techniques which also can help us to evaluate the extent of the disease based on amount of proliferation, and presence of nodules, both cartilaginous and calcified. The terms synovial chondromatosis and synovial osteochondromatosis have been used for the same condition, but the term synovial osteochondromatosis has become less common because the lesions are not only unrelated to osteochondromas, but they are also not ossified. Chondromatosis is a benign metaplastic chondroid proliferation that is distinct from the other causes in that it arises from primary chondrometaplasia of the synovium. Synovial chondromatosis most often affects the knee, while it occurs rarely in the shoulder girdle. Thus, differences of incidence, location of occurrence, clinical symptoms, radiographic findings, and results of surgical resection between primary and secondary chondromatosis occurring in the shoulder remain unclear. Having knowledge of the existence of this disease in the shoulder joint will help orthopaedic surgeons to diagnose and treat this rare condition better in patients.
Clinical Message
Synovial Chondromatosis of the Shoulder Joint is a very rare disorder, although the exact incidence remains unclear. This case report aims to provide orthopaedic surgeons knowledge on when to suspect synovial chondromatosis in a patient coming with chronic shoulder pain, how to workup the patient and most importantly how to treat the patient. This case report aims to reduce the incidence of undiagnosed / misdiagnosed cases of Synovial Chondromatosis of the Shoulder who are in chronic pain because of not getting the proper treatment.