Introduction
Clubfoot, or congenital talipes equinovarus varus (CTEV), is one of the most prevalent foot deformities in children, with a reported prevalence of 0.5-2 occurrences per 1000 live births.1 Approximately 20% of people with CTEV also have additional congenital defects.2, 3 In approximately 50% of instances, bilateral deformity is observed, with a male to female ratio of 2:1. The injured foot is most often the right foot in unilateral situations.4 There is a 10% probability that a second child of parents who already had one impacted by CTEV will also be affected.5
While there is ongoing dispute on the precise etiology, there is general agreement that there are several genetic and environmental risk factors that contribute to the disease's clinical manifestations to differing degrees.6 Maternal diabetes and smoking are two environmental factors that are most strongly linked to clubfoot. In utero location and maternal alcohol use have also been mentioned in the literature.7, 8, 9 Even though it's unclear what precise gene is altered, genetics probably plays a part. Research on monozygotic twins has revealed a 33% concordance compared to a 3% concordance in dizygotic twins.10
The four parts of CTEV are the equinus with associated soft tissue anomalies, the forefoot adductus, the hindfoot varus, and the midfoot cavus. Congenital talipes equinovarus can be classified as "idiopathic" if it occurs in isolation, or as "syndromic" if it manifests in conjunction with other characteristics as part of a genetic condition.
In the last few decades, the Ponseti approach for treating children with CTEV has become widely accepted in the orthopaedics community worldwide. The approach is tried-and-true, has a strong track record, and produces solid long-term outcomes. The traditional regimen for this kind of treatment entails weekly intervals of plaster casting and a series of operations aimed at gradually correcting the deformity. Over the course of 4-6 weeks, there are typically 4-6 casts in this serial casting. To avoid recurrence, the feet abduction brace keeps the repaired foot in place until the child reaches four years old.11, 12, 13, 14 It was proposed that the Ponseti method's expedited protocol be used to reduce the length of time the traditional procedure must be administered. The fundamental of manipulations and plaster casting remains the same but is changed twice or three times per week.15, 16, 17, 18, 19
This study aimed to determine the effectiveness of the accelerated Ponseti method in the treatment of cases with clubfoot deformity and compare it with conventional one in Tezpur medical college.
Materials and Methods
Type of study-Hospital based prospective study.
Place of study-Tezpur medical college and hospital.
Duration of study- 1 year.
Patients selection.
Inclusion criteria
All patients attending orthopaedics OPD and casualty at Tezpur medical college with
Sample size
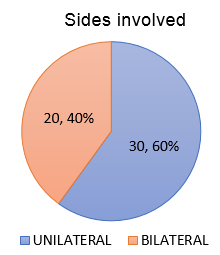
Cases 30 unilateral cases and 20 bilateral cases so total of 70 feet.
The patients were randomized by the authors to either the accelerated one (Group 1) or the standard protocol (Group 2) of Ponseti method in an alternating consecutive manner. The first case was included in Group 1, the second case was included in Group 2, the third case was included in Group 1, and so on). Randomization occurred at the patient level, with both feet being treated using the same method in case of bilateral feet deformity. Informed consent from the patient's parents was obtained before starting the treatment.
Procedure [Figure 1]
The Ponseti procedure involves correcting the clubfoot deformity using a particular technique, and then applying a plaster cast with the foot in the repaired position. In most cases, a percutaneous tenotomy of the Achilles tendon is performed before the final cast in order to achieve total repair. Using a foot abduction orthosis for bracing is essential to reduce the likelihood of the deformity relapsing. The method begins with the Ponseti manipulation and consists of the following steps:
Identify the head of the talus by palpation.
To correct the cavus deformity and restore a normal-appearing arch, supinate the forefoot.
Using the lateral head of the talus as the fulcrum and keeping the reduction of the cavus deformity, abduct the forefoot with the vector of force parallel to the sole of the foot.
This manipulation is followed by the application of an above-the-knee cast with the foot in the corrected position.
The manipulation and casting steps are repeated every 5 to 7 days until the foot is abducted approximately 50° from the frontal plane of the tibia.
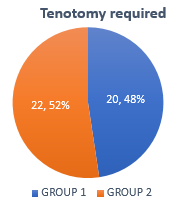
After achieving complete abduction of the foot with the procedures, a percutaneous tenotomy of the Achilles tendon is required in the majority of patients (60–90%) to address the residual ankle equinus.
The final cast is applied and worn for three weeks.
Following the removal of the last cast, the patient is treated for three months by wearing bracing with a foot abduction orthosis for twenty-three hours a day. Bracing is advised until the child is 4 to 5 years old, including at night and during naps. After applying two or three casts, the cavus deformity is removed using a straightforward placement maneuver. The midfoot adduction deformity, the hindfoot varus, and the subtalar component of the equinus deformity are all corrected concurrently when the forefoot is abducted in the plane of the sole of the foot with the head of the talus acting as the fulcrum. After full abduction is obtained, the cavus, adduction, and subtalar varus and equinus deformities are all completely corrected. The only residual deformity is the ankle equinus. Most feet require a percutaneous tenotomy to fully correct the ankle component of the equinus. Tenotomy can be done without any sedation as an outpatient surgery using a local anaesthetic. Tenotomy is not required if the foot can be dorsiflexed to a position greater than 15° (without midfoot breach). Nearly all idiopathic clubfoot can be completely corrected with this procedure in 4–7 sessions.
Results
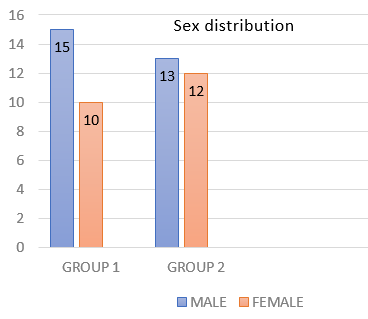
In our study, out of the total 50 cases, 20 cases were bilateral and 30 were unilateral [Figure 2]. The mean age at presentation was 18 days (7 to 48) in group 1 and 26 days (10 to 55) in group 2. There were 15 male patients (60%) and 10 females (40%) in group 1, and 13 male patients (52%) and 12 female patients (48%) in group 2. [FIGURE 3] The mean Pirani score at the beginning was 5.5 (4.5-6) in group 1 and 5.0 (4-6) in group 2. 20 patients (80%) in group 1 underwent tenotomy after correction of cavus, adduction and varus, whereas 22 patients (88%) in group 2 required tenotomy.[FIGURE 4] Mean duration of treatment from the first cast to tenotomy in group 1 was 19.25 days and in group 2 was 45.25 days, which was statistically significant (p<0.001).In our study, accelerated group patients needed 6 plasters per foot for correction and standard group 6.25 plasters per foot. The Pirani score at the end of three-week plaster post tenotomy showed no significant difference (Pirani score=0-0.5) between the two groups.
Comparison of characteristics between randomized groups have been shown in Table 3.
Table 1
Pirani score at different stages of treatment shown on Table 2:
Table 2
Relapse rate in both groups and need of second tenotomy shown in Table 3:
Discussion
Currently, the most widely utilized approach for managing CTEV is the Ponseti method. Weekly manipulation and casting, the classic Ponseti procedure, is low-cost, has a short learning curve, and has produced great outcomes in both short- and long-term studies. Using the head of the talus as a fulcrum to extend the constricted ligaments and maintain the stretch with serial casting, Achilles tendon tenotomy, and bracing—foot abduction brace—is a specialized manipulation technique known as the ponseti technique. Morcuende et al. conducted the most extensive trial over an 11-year period, serially manipulating the cast every 5 days in order to achieve a successful correction with or without negligible side effects.16 Our aim was to establish the effectiveness of a twice-weekly accelerated protocol vis-à-vis the standard protocol in our population cohort.
In both groups, there was a marginally greater male predominance in our study. This is also the outcome of research conducted by Ullah et al. and Solanki et al. 19, 17
The expedited group needed 19.25 days, while the traditional group needed 45.25 days for the plaster correction. This difference was statistically significant (p<0.001). The outcome of numerous investigations was the same. Sharma et al.,15 Harnett et al.,14 and Morcuende et al.16
In the expedited group, the mean number of castings needed was 6, while in the regular group, it was 6.25. The figures were 4.88 and 5.16 in the research by Elgohary and Abulsaad20 and 4 and 4 in the study by Harnett et al. 14
In our study, tenotomy rate between the two procedures does not differ significantly, though it is slightly higher in accelerated Ponseti method.
This might be due to slightly higher initial Pirani score in accelerated group as mentioned by Mageshwaran et al. (2016) 21
The limitations of the study includes the study sample was small and the follow up is done only till one year.
Conclusion
There are a number of social and economic problems in a nation like India where parents must travel great distances to bring their children for serial casting. It has become necessary to reduce the amount of time needed for deformity repair, given the psychological and financial strain that traveling great distances to the treatment center places on the family of the patient with club foot. When accelerated Ponseti casting is used instead of standard casting, treatment days are significantly shortened while follow-up outcomes remain comparable.
By lowering the number of missed work days and the overall cost of the trip, accelerated casting can considerably lessen the financial strain on the underprivileged patients.
Authors’ Contributions
Prof Dr Chinmoy Das has made substantial contributions to the concept and design, and is the main author. Dr Swapnaneel dutta and Dr Somesh Saha have been involved in the drafting of the manuscript and revised it critically for important intellectual content. All authors have agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.