Introduction
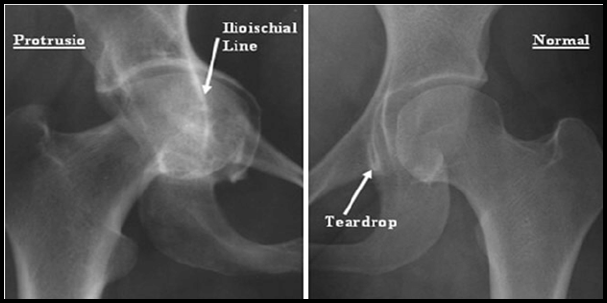
Protrusio acetabuli is a central acetabular defect resulting from migration of femoral head medial to Kohler’s line.1 This results in medialization of the center of rotation (COR) of the hip. Primary Total Hip Replacement (THR) in such situations can be technically demanding due to associated significant medial and proximal migration of the center of the joint, deficient bone medially2 and reduced bony support to the acetabular component peripherally.
Cemented total hip arthroplasty resulted in promoting bone lysis and implant loosening, however, uncemented total hip arthroplasty with impacted morselized autograft with a porous coated cementless acetabular component provided a biological solution to bone deficiency and long-term fixation in arthritic hips with protrusio. 3, 4
Functional outcome of uncemented total hip arthroplasty was evaluated by Harris hip score pre & post operatively in the cases. 5, 6
Materials and Methods
This is an Observational study conducted at R.D. Gardi Medical College and associated CRGH, Ujjain (M.P.), between period August 2019 to July 2021 on a total of 20 cases who are fulfilling the Inclusion criteria.
All the patients included in the study were functionally evaluated by Harris hip score pre operatively along with an X-Ray of pelvis with both hips.
Surgery was performed with the patient in the lateral position.
All the patients were operated with uncemented total hip replacement by a standard posterior (Southern Moore) approach.
Same type of implant was used in all the patients.
Dislocation of hip was challenging due to deepened acetabulum and medial displacement of the femoral head. It was facilitated by an extensive capsulotomy, along with simultaneous and sustained gentle traction and rotation.
Removal of posterior osteophytes before dislocation also helped.
Adductor tenotomy performed in cases with excessive adductor tightness.
In cases of difficult dislocation, femoral neck was resected in situ and the femoral head was excised piecemeal.
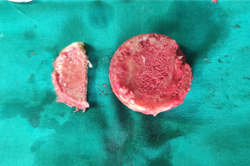
Normally, before neck osteotomy, dislocated femoral head was cut into slices with a power saw.
The bone slices were then morselized into 8mm-10mm sized pieces using a bone cutter.
After neck osteotomy, acetabular floor prepared while avoiding penetration of a soft, deficient medial wall until a bleeding bony surface was obtained.
Acetabular periphery reamed using large sized reamers initially.
The morselized graft was then introduced into the prepared acetabulum and impacted against the floor using hemispherical impactors.
Reverse direction reaming was done to further impact and set the graft in the floor of acetabulum.
An acetabular cup trial was inserted to ensure good peripheral fit and more than 50% contact with the host bone.
Finally, the chosen acetabular component was impacted into place.
Post-operative protocol
Post operative AP X-Ray view of the operated hip obtained.
Abduction pillow used during the sleeping time for 7-10 days post-operatively.
Active and active assisted range of motion exercises started within the first 24-48 hrs.
Partial weight bearing with a walker was advised upto 3 months until bone grafts appeared to be incorporated in xray.
Full weight bearing started at 3 months.
Results
Maximum patients (10) were in the age group of 50-60 years.
With a female predominance of 8 patients (53%), and 7 male patients (47%).
10 patients had unilateral involvement whereas 5 patients had bilateral involvement.
The most common etiology was found to be Rheumatoid Arthritis (10) followed by Idiopathic (7) followed by Ankylosing Spondylitis (3).
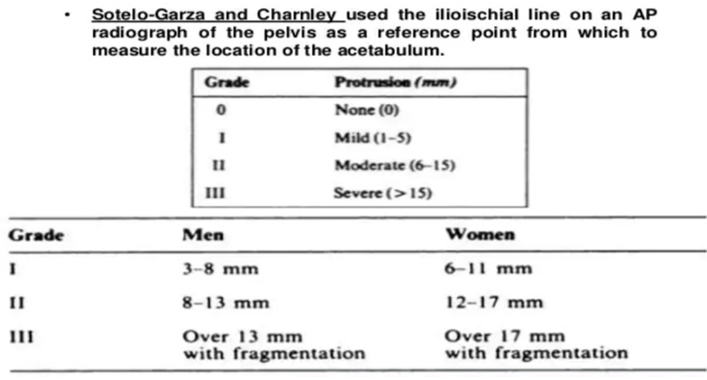
4 had mild, 7 had moderate and 9 had severe grades of protrusio.
The operation time ranged from 60 to 120 minutes (mean= 79.4 ±14 mins).
The blood loss ranged from 200-400 ml (mean=262±36 ml).
The mean preoperative Harris Hip Score was 48 which improved to 90 at the latest follow-up.
10 hips (50%) had excellent,8 hips (40%) had good, and 2 hips (10%) had fair results. There was no dislocation.
The mean acetabular inclination angle was 44.2° (range 39°-47°).
The distance from the femoral head center to Kohler’s line improved from 17.98 preoperatively to 20.36 post operatively).
Table 1
|
Harris hip score |
|||||
|
S.No. |
Pre-Op |
6 weeks |
03 Months |
06 Months |
01 Year |
|
1 |
48.4472 |
68.0364 |
76.2004 |
84.6428 |
90.0852 |
Discussion
Study by Mullaji et al suggested that the use of impacted morselized autograft in conjunction with porous coated cementless acetabular component restored hip biomechanics after an intermediate duration follow up. 30 primary THR’s were conducted with a 4.2 year follow up which showed excellent outcome in 90% patients, fair in 7% patients and poor in 3% patients. 9 Study by Atanu et al showed that using only cement for acetabular reconstruction in protrusio acetabuli has had unacceptably high rates of recurrence, with components migrating into the acetabulum and occurrence of thermal necrosis of the thinned out medial wall due to heat polymerization of the cement. 10 These were some of the factors responsible for poor outcome.
Table 2
Comparison of results of different techniques used to treatacetabular protrusio with primary THR in literature published since 2000
|
Studied |
No. of Hips |
Mean age at surgery (Years) |
Techmique |
Survival of acetabular component |
|
Mullaji et al 9 |
30 |
46 |
Impacted morselissed bone graft with cement less cup |
100% at 4.2 years |
|
Garcia Cimbrelo et al. 11 |
148 |
54 |
Cemented polyethylene component |
79% at 16 Years |
|
Perwira et al 12 |
23 |
62 |
Impacted morselissed bone graft with cementless component |
100% at 7.8 years |
|
Rssenberg et al 13 |
36 |
53 |
Impacted bone graft with cemented component |
90% at 12 years |
|
Krushell et al 14 |
29 |
66 |
Impacted morselissed bone graft with dual geometry cementless component |
100% at 2 years |
|
Current study |
9 |
54 |
Impacted, morsellised bone graft with cementless cup |
100% at 2 yeras |
Conclusion
We treated 20 cases of Protrusio Acetabuli of mild, moderate and severe grades by Sotello-Garza and Charnley by uncemented total hip arthroplasty using morselized autograft. It helps in restoring biomechanics of hip joint and preventing recurrence of protrusio. We observed fair, good and excellent functional outcomes in our patients. There was no evidence of progression of protrusio or socket loosening in any of our cases. Osteolytic lesions were also not encountered by us in our study. All bone grafts united within 4-6 months after surgery and continuous trabecular bone that grew through the host bone and the bone graft was apparent. But a larger sample size and a longer follow up are required to ascertain this fact.