Introduction
Nonunion or Delayed-union of fractures occurs in about 5% to 10% of long-bone fractures.1 Nonunion is defined as a fractured bone that has not completely healed within 9 months of injury and that has not shown progression towards healing over 3 consecutive months on serial radiographs.2 A delayed union is generally explained as a failure to have bony union by 6 months after having fracture. In other words, it is the condition when fractures take longer than expected time to heal. Both, delayed and nonunion are serious complications which prolong patient morbidity, loss of productivity, time lost from work and economic hardship.
Teriparatide (TPTD), also called as rPTH(1-34) is the recombinant parathyroid hormone analog containing first (amino terminus) 34 amino acids of PTH (Parathyroid Hormone). It is considered the as the bioactive fragment of PTH delivering the same physiological effects.3 Teriparatide when given in the form of pulse therapy as 20mcg daily subcutaneous injections acts as an anabolic agent and increases bone mass by predominant activity on osteoblasts. Presently, Teriparatide is approved by USFDA for treatment of postmenopausal women with osteoporosis at high risk of fracture, increase of bone mass in men with primary or hypogonadal osteoporosis at high risk for fracture and treatment of men and women with osteoporosis associated with sustained systemic glucocorticoid therapy at high risk for fracture.3 Because of its osteoanabolic effect, Teriparatide has always been of clinical interest for its potential role in fracture healing. In fact, it is being used clinically worldwide for fracture healing as an off label indication. The purpose of this review is to summarize the accumulating preclinical and clinical evidence for role of TPTD in accelerating fracture healing in various conditions like conservative management of fractures, vertebral fractures, non-unions, delayed unions and atypical femoral fractures.
Mechanism of fracture healing & role of TPTD
After a fracture, healing takes place in two ways: primary healing in which the first step is union of the bone cortex which is followed by anatomic restoration with rigid fixation, and secondary healing, in which periosteum and external soft tissues lead to formation of callus.4Secondary healing is more common and it involves a combination of endochondral and intramembranous ossification. The first step is formation of hematoma leading to influx of inflammatory cells which secrete cytokines like platelet-derived growth factor, bonemorphogenic protein and transforming growth factor beta.4, 5, 6, 7 Along with this, periosteal mesenchymal stem cells activation and angiogenesis occurs.8 After this, undifferentiated mesenchymal stem cells get differentiated in to chondrocytes and osteoblasts which lead to ossification of endochondral (soft callus) and intramembranous(hard callus), respectively. In the soft callus, chondrocytes after differentiation produce type X collagen and mineralize, so that calcified cartilage is replaced by woven bone. On the other hand, intramembranous bone formation in the hard callus immediately begins after the occurrence of fracture without initial formation of cartilage.4, 8 These processes utilize similar signaling pathways as that of normal bone healing, including Wnt, transforming growth factor beta,bone morphogenetic proteins, Indian hedgehog signaling and insulin-like growth factor.8 After primary bone formation, osteoclastic bone resorptionand laying down of mature lamellar bone takes place in remodeling phase. 4, 6, 8
Teriparatide treatment enhances and accelerates the skeletal repair process via a number of mechanisms including effects on mesenchymal stem cells by regulation of osterix, angiogenesis, chondrogenesis, bone formation and remodeling. 9
Preclinical evidence
Numerous studies using small animal models have demonstrated that PTH enhances fracture healing. In 1999, Andreassen et al. showed that PTH increased callus formation and ultimate load to failure for tibial fractures in adult rats. 10 Intermittent administration of PTH(1-34) at 60 and 200 mcg doses produced increases in callus volume of 42% and 72% respectively and increased ultimate load to failure by 132% and 175% respectively after 40 days. In the same year, Holzer et al. found histological evidence of increased callus area and improved bone strength after daily PTH(1-34) administration in rats. 11
Formation of fibrotic tissue is one of the important factors which lead to non-union of fractures. TPTD in murine cranial allogeneic bone grafts has shown to induce small diameter vessel formation as early as 1st week of surgery. This modulation of neovascularization reduces fibrosis and scar tissue formation leading to superior bone graft integration by facilitating osteogenesis. 12
In a study conducted on murine cranial window model, Zhang L et al. demonstrated efficacious non anabolic effect of TPTD causing mast cell inhibition leading to suppression of arteriogenesis and fibrosis which ultimately improved healing. 13
Kakar S et al. conducted a preclinical study on 8-wk-old male C57Bl/6 mice in whom closed femoral fractures were inflicted. Effect of 14 days daily systemic injection of TPTD 30mcg/kg was compared to normal saline. The TPTD group demonstrated threefold greater increase in chondrogenesis relative to osteogenesis during the repairing process. Chondrocyte hypertrophy was also seen early in TPTD treated group. TPTD also increased the expression of Wnts 4, 5a, 5b, and 10b and increased levels of unphosphorylated, nuclear localized beta-catenin protein, which play a significant role canonical Wnt signaling. All these molecular and cellular changes led to larger callus cross-sectional area, length, and total volume in TPTD group as compared to control. 14
Clinical evidence: Acceleration of fracture healing
An observational cohort of 145 patients with radiographically documented fractures of various sites including spine, ribs, pelvis, hip, femur, tibia, foot, subtalar fusion, humerus and wrist was presented in 55th Annual Meeting of the Orthopaedic Research Society. All patients tolerated daily dose of TPTD with no complications. 97.2% of patients had pain resolution at fracture or fusion site within 12 weeks of starting TPTD. Point worth noting was that 88% of the total cohort had either failed previous fracture healing, and who presented with their current fracture as a delayed union or nonunion, or were elderly and high risk candidates for surgical intervention for their fracture sites. 93% patients demonstrated complete healing and 4% demonstrated partial radiographic healing. 15
A retrospective analysis of 60 patients who underwent closed reduction and internal fixation with proximal femoral nail for unstable fracture when compared to 52 patients who additionally took daily SC TPTD showed that TPTD significantly increased Harris hip score and decreased VAS pain scores. In addition, the frequency of patient reported postoperative complications was also less in TPTD treated group. 16
In a randomized, multicenter, active controlled 78 week trial, Aspenbertet al. compared the effects of TPTD and risedronate on recovery after pertrochanteric hip fractures. The therapy was initiated in low trauma pertrochanteric hip fractures within two weeks of fixation. Data of 171 patients was analyzed out of which 86 and 85 patients were on TPTD and risedronate therapy respectively. The time taken to complete TUG test (Timed Up-and-Go test) was shorter in TPTD group as compared to risedronate group at 6, 12, 18 and 26 weeks (differences of -5.7, -4.4, -3.1 seconds, respectively). TPTD group also reported significantly less pain (VAS) at 12 and 18 weeks. Other fracture recovery outcomes like SF-36 score, Charnley hip pain score, ability to walk or use of walking aids were similar in both the groups. 17
In another randomized, pilot study planned to evaluate the effect of brief administration of TPTD on lower extremity stress fractures in 13 patients, TPTD increased bone formation biomarkers N-terminal propeptide of type I procollagen (P1NP) and osteocalcin as compared to placebo.Peripheral quantitative computed tomography showed that TPTD treated patients had a larger cortical area and thickness at the weight bearing tibial site as compared to placebo. Improvement or healing of stress fracture as seen on MRI was seen in 83.3% and 57.1% cases in TPTD and placebo group respectively. 18
Huang TW et al. published a retrospective study assessing the effect of TPTD on fracture healing and early functional recovery in osteoporotic intertrochanteric fractures. They found a significant short time-to-union in TPTD treated patients as compared to patients who received only vitamin D and calcium. Quality of life as measured by SF-12 PCS (short-form health survey[SF]-12 physical component summary[PCS]) and pain scores were also better in TPTD group at 3 & 6 months. TPTD treated group also reported less mortality and complications. 19
Ochi K et al. treated an elderly woman of 74 year who had rheumatoid arthritis and total knee replacement. Her periprosthetic fracture did not unite despite undergoing internal fixation and bone grafting twice. She was started on once weekly TPTD leading to successful bone healing in 6 months. 20
Kim Y et al reported the outcome of three cases of femoral insufficiency fractures after giving TPTD. TPTD increased abundant callus formation at fracture site as early as at 2 weeks. Callus formation was also seen around cortex with a ‘cloud-like’ appearance. Remodeling of the callus was part of normal fracture healing process. 21
Huang TW et al. in a retrospective study demonstrated that TPTD as an adjuvant to dynamic hip screw fixation (DHS) in unstable pertrochanteric fractures significantly improved fracture healing time. It also significantly improved overall mobility scores and pain scores at 3 and 6 months as compared to patients who received DHS fixation only. This reduction in healing time can be very important in elderly cases wherein it can lead to early return to daily activities and reduction in morbidity and mortality. 22
Multiple case reports of fracture healing with TPTD have been reported in various conditions like osteogenesis imperfect, 23 charcot arthropathy, 24 metatarsal stress fractures, 25 subtrochanteric stress fractures, 26 hypophosphatasia. 27
TPTD evidence in vertebral fractures
Vertebral fractures are very common in osteoporosis and a good response to TPTD is expected as it significantly improves the BMD (Bone Mineral Density) in lumbar spine which have a large proportion of trabecular bone. 28
Iwata A et al. did a retrospective study to compare effect of TPTD and bisphosphonates on healing of osteoporotic vertebral compression fracture. The analysis of 98 patients’ data showed that the time to union was reduced significantly by TPTD and at 6 months, the union rate in TPTD group was 89% as compared to 68% in bisphosphonate (BP) group. There was no requirement of any surgical intervention at the fracture site in TPTD group unlike BP group in which 2 out of 60 patients underwent surgical treatment for symptomatic non-union or vertebral collapse. 29
In another study, Yang DH evaluated conservative treatment with TPTD in 12 cases of osteoporotic vertebral compression fractures. Within one month of therapy, analgesics were withdrawn in all patients, VAS pain score was reduced from 8±2 to 1±2. The mean BMD and bone turnover markers viz. P1NP and beta CTX were increased in 6 months. There was an insignificant reduction in heights of vertebral fractures over 6 months. No new fracture or adverse event was reported in any case during the study. 30
TPTD evidence in non-union
In a prospective study conducted on 32 patients with non-union of long bones, Teriparatide was reported to lead to definitive healing in 95% of cases. The mean duration to achieve first sign of healing was 7.3±1.5 weeks. 31
Several published case reports have suggested the beneficial effect of Teriparatide on non-unions. Chintamaneni et al. reported on a 67-year-old male who sustained a fracture of the body of the sternum as a result of a motor vehicle accident. This subsequently failed to heal resulting in a painful atrophic non-union. A trial of 20 mcg per day of Teriparatide was initiated and showed significant healing of the non-union within 3 months and complete healing and symptomatic resolution after 9 months. 32
In a recently published case report, TPTD treatment led to successful union in a case of femoral fracture nonunion even after 1 year of autogenous bone grafting in a 45-year-old man.33 In another case with non-union of post traumatic type II odontoid fracture in an elderly woman, treatment with TPTD led to resolution of symptoms and complete fusion in 12 weeks. 34
Uemura T et al. reported two smokers with nonunion after ulnar shortening osteotomy and fixation with non-locking plate for ulnar impaction syndrome. Within 4 weeks of TPTD therapy, partial bone union could be observed on x-rays and successful healing was achieved at 6 and 10 months. 35
A case report of a 74 year old woman with rheumatoid arthritis who incurred a peri-prosthetic fracture after undergoing total knee arthroplasty was reported by Ochi K et al. The fracture did not unite despite internal fixation and bone grafting twice. TPTD was initiated once weekly which led to successful bone fusion. 36
Bedner DA reported an odontoid fracture type III in a 70-year woman who was on steroids. Realignment of the fracture and a properly fitted Miami-J collar failed to heal the fracture in 3 months. After initiation of TPTD, fractured healed partially in 3 months and completely in 6 months as confirmed by CT scan. 37
Giannoti S et al. reported a case of right distal metaphyseal femoral fracture after total knee arthroplasty for which she underwent open reduction and internal fixation with lateral femoral locking plate. The fracture went into non-union after 7 months for which she was given TPTD following which, bone bridges were seen after next 2 months and the fracture completely healed in 3 months. 38
One of the earliest case reports on sternal non-union was published as early as in 2010 by Chintamaneni S et al. wherein TPTD led to successful union. 39
TPTD evidence in delayed union
Some data have emerged over the time regarding benefits of TPTD in delayed union fractures.
Bukata et al. reported a series of 145 patients with fractures of the spine or other extremities that were treated with 20μg of TPTD. Half of the patients in this study demonstrated delayed fracture healing and 88% had failed a previous attempt at union, presented with a non-union, were elderly or had significant medical comorbidities. Regardless of fracture site, 141 people reported resolution of pain at the fracture site within 12 wk of starting Teriparatide and the fracture united in 93%. 40
Ilko Kastirr et al. performed plate osteosyn thesis of the fibula and tibia in a 49-year-old man who incurred a distal lower leg fracture in a skiing accident. At seven months, diagnosis of oligotrophic delayed union was given when there was insufficient consolidation of the fracture. The patient could place limited weight on the limb which was leading to pain. As patient did not consent for further surgery, TPTD was given which led to osseous consolidation of the fractures in 4 months. 41
TPTD evidence in atypical femoral fractures (AFF)
AFF have been defined by ASBMR (American Society for Bone and Mineral Research) as fractures satisfying all major features viz. location in the subtrochanteric region and femoral shaft, transverse or short oblique orientation, minimal or no associated trauma, a medial spike when the fracture is complete, and absence of comminution. In addition, the minor features might be associated like cortical thickening, a periosteal reaction of the lateral cortex, prodromal pain, bilaterality, delayed healing, comorbid conditions, and concomitant drug exposures, including BPs, other antiresorptive agents, glucocorticoids, and proton pump inhibitors.42 The healing of atypical femoral fractures is often delayed. TPTD has been reported to enhance AFF healing in various studies.
In a retrospective study done by Miyakoshi et al., data of surgically treated AFF was analyzed to evaluate the effect of adjuvant TPTD. TPTD significantly reduced the time to fracture healing (5.4±1.5 months) as compared to patients who did not receive TPTD (8.6±4.7 months). TPTD group also reported significantly less frequency of delayed union or non-union. 43
In another retrospective observational study on patients with recent low trauma fracture after prolong use of BPs, 11 out of 21 patients had completely healed fractures after completing Teriparatide course (18-24 months). Teriparatide was also reported to improve thigh pain. 44
Kim JT et al. demonstrated the effect of adjuvant TPTD in 13 surgically treated cases of AFF, periprosthetic femoral fracture and femoral non-union. Within a year of starting TPTD, twelve of these thirteen fractures healed both clinically and radiologically. The median time to heal radiologically and clinically was 5.4 and 5.7 months respectively. The study concluded that adjuvant TPTD with stable fixation for the challenging fractures of femur results in satisfactory outcome. 45
A 63-year-old woman with AFF due to long term alendronate therapy was successfully treated with TPTD. There was remarkable improvement in pain and tenderness within a duration of one month. 46
In a recent study conducted by Greenspan SL et.al, on 13 patients with bisphosphonate associated AFF, immediate administration of TPTD therapy led to superior healing at 6 and 12 months as compared to patients in whom TPTD administration was delayed by 6 months after incurring AFF. 47
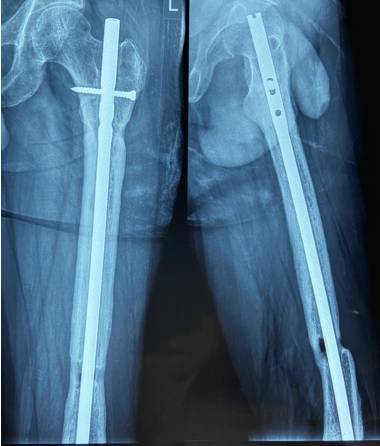
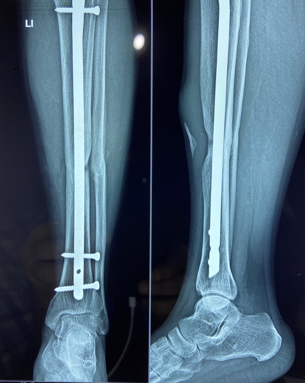
In a series of delayed union with internal fixation over 47 patients regardless of the fracture sites communition or inadequate fixation, had union in all patients including a case of infected nailing of femur. These patients had reported to Dr. S S Jha three to seven months after internal fixation at other centers. None of these patients were willing to submit themselves for further surgical intervention. Teriparatide 20mcg daily through subcutaneous route was started in all patients with adequate supplementation of vitamin D and calcium. Evident radiological bony union was perceptible after three months with clinical improvement in the initial presenting symptoms of the patients and the osseous consolidation was invariably observed radiologically within four to six months. It was only in six patients that Teriparatide was continuously used for one and half years for reasons of general debility, elderly age and osteoporosis. Radiographs of three difficult cases are being displayed from the series.
Case 3(Figure 12)
Conclusion
The available preclinical and clinical evidence indicates that TPTD plays a significant role in promoting fracture healing in conservative management of fracture healing as well as in cases of delayed and non-union. Most of the published data todaycomprises of case reports, case series and retrospective studies. Need of the day is to conduct large, prospective, randomized controlled trials to generate quality evidence so that authorities can be approached for approval of TPTD in fracture healing.