- Visibility 51 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijor.2020.018
-
CrossMark
- Citation
How does medial compartment osteoarthritis of knees respond to proximal fibular osteotomy at one year ? – A prospective analysis of 26 knees
- Author Details:
-
Ajay SS *
-
Anil Gowtham Manivannan
-
Madhan Jeyaraman
Introduction
Knee osteoarthritis (OA) is a chronic, progressive degenerative disease with joint pain, stiffness, and deformity.[1] Knee OA is a common joint disease, with an incidence of 30% of the population older than 60 years.[2], [3] Medial compartment OA is very common, almost the commonest non-communicable disease in India, and around 50% of the Indian Population have Varus knees.[4], [5] Knee varus deformities, characterized by a mechanical femorotibial axis of less than 180° on full-leg standing anteroposterior (AP) radiographs and narrowed medial joint space, are common in patients with knee OA.[6], [7]
High tibial osteotomy and total knee arthroplasty are the two commonly used methods for treating knee OA.[8] Total knee arthroplasty (TKA), which aims to relieve pain and improve joint function and mobility, proximal fibular osteotomy (PFO) is the main surgical alternative in this patient population.[9] However, TKA is expensive and complex and some patients need a second knee revision after the first surgery.
Non-uniform medial and lateral supports in varus knees is because of osteoporotic tibia medially and three cortex supports laterally. This leads to the non-uniform settlement which may result in the load from the normal distribution, shifting farther medially to the medial plateau and consequently lead to knee varus, aggravating the progression of medial compartment OA of the knee joint.[10] In this study, we analyzed the effect of PFO in the medial compartment osteoarthritis of the knee joint.
Materials and Methods
The study was conduction after obtaining institutional ethical committee clearance.
Inclusion criteria
The patients with medial compartment osteoarthritis with varus knee, grade 2 and grade 3 OA knee in Kellgren and Lawrence classification, good lateral joint space in weight-bearing X-ray films, and age more than 20 years were included in the study.
Exclusion criteria
The patients with severe osteoarthritis, inflammatory arthritis, genu valgus deformity, acute major trauma, grade 0, 1, and 4 OA knee in Kellgren and Lawrence classification, lateral joint space less than medial joint space in weight-bearing X-ray films, and lateral compartment osteoarthritis of the knee were excluded from the study.
Surgical technique
The surgery was performed with the patient in the supine position under spinal anesthesia with antibiotic cover. The fibular head was marked and the osteotomy site was determined to be 7 to 9 cm from the head of the fibula.[9], [11] The rationale behind choosing this level of osteotomy is to avoid injuring the common peroneal nerve. A 5-8 cm lateral incision was made overlying the chosen site of osteotomy and dissection was carried out through the skin and subcutaneous tissues. The peroneus and soleus muscles were then separated to expose the periosteum of the fibula which was then incised and a 1.5 to 2 cm of the fibula was then resected with the help of an oscillating saw after placing a few drill holes at the osteotomy site. After ensuring hemostasis and giving wound wash, the closure was done in layers and sterile dressing and compression bandage applied. All patients were encouraged to stand and walk on the same evening of surgery and were discharged on the third postoperative day after the first wound inspection
All the patients were followed up at 1, 3, 6, and 12 months. Patients were analyzed for any complications and their functional outcome was compared with their previous status. The patients were evaluated objectively by weight-bearing radiographs and knee pain was assessed using a visual analog scale (VAS), and knee ambulation activities were evaluated using the American Knee Society score (KSS) preoperatively and postoperatively.
The descriptive statistics were reported as mean (SD) for continuous variables, frequencies (percentage) for categorical variables. Data were statistically evaluated with IBM SPSS Statistics for Windows, Version 24.0, IBM Corp, Chicago, IL. The paired student t-test was used to analyze the significance of the outcomes analyzed post-intervention. P<0.05 was considered significant.
Results
The proximal fibular osteotomy was performed in twenty-six knees of twenty patients with a minimum age of 45 and a maximum age of 68 and the average age is 56.5 years. The majority of the patients were from the age group of 50-65 years which accounts for 75% of patients in our study. The youngest patient was 47 years of age and the oldest patient was 68 years. The mean age was 57.15 years. There was a female predominance in our study accounting for 65% of the total patients.
In our study, the mean pre-op KSS score was 33.5 which has improved post-operatively to 83.57 at one-year follow-up, which falls under excellent result (p=0.002). VAS score had significantly reduced postoperatively at one-year from mean 6.3 to 2.8 indicating that the patients got relieved of pain (p<0.01) as shown in [Table 1].
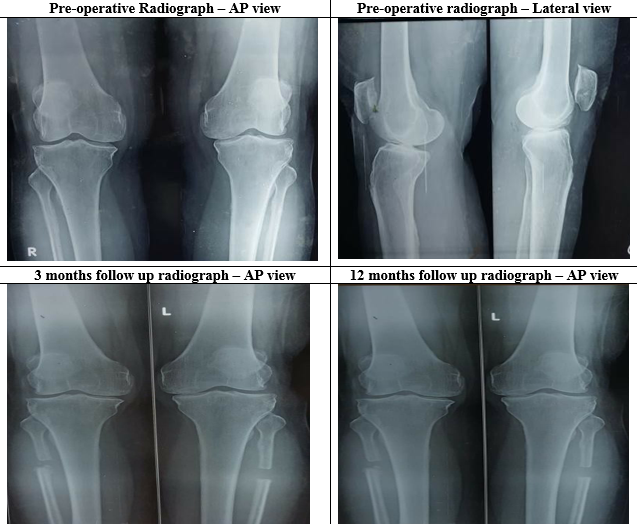
The medial joint has opened up from a mean of 1.15 mm to 3.4 mm and lateral joint space has reduced from 5.69 mm to 5.3 mm as shown in [Table 2] and illustrated in [Figure 1]. In our study, the ratio of medial joint space to lateral joint space has improved significantly from pre-op 0.20 mm to 0.56 mm post-op, indicating the opening up of medial joint space.
|
|
Frequency |
Mean |
Minimum |
Maximum |
|
American Knee Society Score (KSS) |
||||
|
Pre-Op |
20 (26 Knee) |
33.5 |
24 |
45 |
|
Post-Op |
20 (26 Knee) |
83.57 |
78 |
90 |
|
VAS Score |
||||
|
Preop |
20 (26 knee) |
6.3 |
5 |
7 |
|
Postop |
20 (26 knee) |
2.8 |
1 |
3 |
|
|
Frequency |
Medial joint space (mean) |
Lateral joint space (mean) |
Ratio (M/L) |
|
Pre-op |
20 (26 knees) |
1.15 mm |
5.69 mm |
0.20mm |
|
Post-op |
20 (26 knees) |
3.4 mm |
5.3 mm |
0.56mm |
Discussion
In this study, a total of 20 cases (26 knees, 6 cases were bilateral) of medial compartment osteoarthritis of the knee were treated with proximal fibular osteotomy. Other surgical options available for the management of medial compartment arthritis of the knee are limited to high tibial osteotomy and uni-condylar knee replacement.
High tibial osteotomy corrects the varus deformity associated with medial compartment arthritis of the knee but it is associated with a longer recovery period and a prolonged period of non-weight bearing walking until the union of the osteotomy site.[12], [13] There can be issues such as recurrence of varus deformity and can also lead to revision to total knee arthroplasty due to persistent pain.[14]
Uni-condylar knee replacement is another procedure in the management of medial compartment arthritis of the knee which has produced mixed results according to various studies in the literature.[15], [16] This procedure could be associated with problems such as poly wear, progression of arthritis, or loosening of components.[17], [18] Certain studies have demonstrated a high rate of revision for uni-condylar knee replacement as compared to a total knee replacement.[19]
In this scenario, there is a need for a procedure that is simple to perform, easily reproducible, gives good functional results, and is associated with a shorter recovery period thereby improving the quality of life of the affected patients. The theory behind the development of medial compartment osteoarthritis suggests that there is an asymmetric load transmitted across both tibial plateaus with more stress being borne on the medial side which eventually becomes lower leading to the development of a varus deformity and arthritic changes occur with degeneration of the articular cartilage.[20], [21], [22] PFO acts by weakening the support laterally, correct the varus deformity, and shifts the stress from the medial to the lateral compartment resulting in alleviation of pain and gives a good functional outcome. [23], [24], [25], [26], [27]
In a study by Yang et al, 150 patients with medial compartment arthritis were followed up for more than 2 years. The preoperative KSS score was 45±21.3 which improved postoperatively to 92.3±31.7. The mean VAS score preoperatively was 7 which significantly decreased to 2 in the postoperative period. They stated that PFO dramatically improves the function of the knee and gives good pain relief.[10]
In a study by Bo Liu et al, they had 84 patients with 111 knees being affected by medial compartment arthritis. The average preoperative VAS score was 7.08±1.41. The average preoperative KSS and functional scores were 49.14±10.95 and 44.97±17.1 which reduced after PFO to 67.77±11.08 and 64.66±13.12 respectively. 51 knees were associated with a satisfactory clinical outcome while 77 knees had a significant improvement.[28]
The only complication noted in our study was the extensor hallucis longus weakness in two patients which eventually got recovered over a period of time. The advantages of PFO over the other procedures make it a simple, safe procedure and cost-effective procedure of choice for medial compartment knee osteoarthritis. If the procedure does not give good results in any situation then the field for performing total knee arthroplasty, later on, is not disturbed. The limitations of our study were involving only a small sample of patients and a relatively short follow-up period. A longer period of follow-up is necessary to evaluate whether the beneficial effects of PFO are sustained over a period of time.
Conclusion
PFO is a promising alternative procedure in the management of medial compartment osteoarthritis of the knee being a simple and cost-effective alternative to the traditional total knee or unicondylar knee replacements. A longer period of follow-up is necessary to evaluate whether the beneficial effects of PFO are sustained over a period of time.
Acknowledgments
Nil.
Conflict of Interests
All authors have declared no conflict of interests.
Conflict of Interest
None.
References
- DJ Hunter, JJ McDougall, FJ Keefe. The Symptoms of Osteoarthritis and the Genesis of Pain. Rheum Dis Clin North Am 2008. [Google Scholar] [Crossref]
- G Peat, R McCarney, P Croft. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001. [Google Scholar] [Crossref]
- CP Pal, P Singh, S Chaturvedi, KK Pruthi, A Vij. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop 2016. [Google Scholar] [Crossref]
- J Bedson, P R Croft. The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskeletal Disord 2008. [Google Scholar] [Crossref]
- B Heidari. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med 2011. [Google Scholar]
- D Qin, W Chen, J Wang, H Lv, W Ma, T Dong. Mechanism and influencing factors of proximal fibular osteotomy for treatment of medial compartment knee osteoarthritis: A prospective study. J Int Med Res 2018. [Google Scholar]
- JJ Cherian, BH Kapadia, S Banerjee, JJ Jauregui, K Issa, MA Mont. Mechanical, Anatomical, and Kinematic Axis in TKA: Concepts and Practical Applications. Curr Rev Musculoskelet Med 2014. [Google Scholar] [Crossref]
- F Dettoni, D E Bonasia, F Castoldi, M Bruzzone, D Blonna, R Rossi. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J 2010. [Google Scholar]
- X Wang, L Wei, Z Lv, B Zhao, Z Duan, W Wu. Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res 2017. [Google Scholar]
- Z Y Yang, W Chen, C X Li, J Wang, D C Shao, Z Y Hou. Medial Compartment Decompression by Fibular Osteotomy to Treat Medial Compartment Knee Osteoarthritis: A Pilot Study. Orthop 2015. [Google Scholar]
- A Vaish, Y Kumar Kathiriya, R Vaishya. A Critical Review of Proximal Fibular Osteotomy for Knee Osteoarthritis. Arch Bone Jt Surg. Arch Bone Jt Surg 2019. [Google Scholar]
- S Sabzevari, A Ebrahimpour, M K Roudi, A R Kachooei. High Tibial Osteotomy: A Systematic Review and Current Concept. Arch Bone Jt Surg. Arch Bone Jt Surg 2016. [Google Scholar]
- P Hernigou, D Medevielle, J Debeyre, D Goutallier. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 1987. [Google Scholar]
- U Cottino, F Rosso, A Pastrone, F Dettoni, R Rossi, M Bruzzone. Painful knee arthroplasty: current practice. Curr Rev Musculoskelet Med 2015. [Google Scholar] [Crossref]
- S Campi, S Tibrewal, R Cuthbert, SB Tibrewal. Unicompartmental knee replacement – Current perspectives. J Clin Orthop Trauma 2018. [Google Scholar] [Crossref]
- A Fiocchi, V Condello, V Madonna, M Bonomo, C Zorzi. Medial vs lateral unicompartmental knee arthrroplasty: clinical results. Acta Biomed 2017. [Google Scholar]
- M Vasso, A Antoniadis, N Helmy. Update on unicompartmental knee arthroplasty. EFORT Open Rev 2018. [Google Scholar] [Crossref]
- M Vasso, K Corona, R D'Apolito, G Mazzitelli, A Panni. Unicompartmental Knee Arthroplasty: Modes of Failure and Conversion to Total Knee Arthroplasty. Joints 2017. [Google Scholar] [Crossref]
- NA Siddiqui, Z M Ahmad. Revision of Unicondylar to Total Knee Arthroplasty: A Systematic Review. Open Orthop J 2012. [Google Scholar] [Crossref]
- N Shakoor, A Dua, LE Thorp, R A Mikolaitis, MA Wimmer, KC Foucher. Asymmetric loading and bone mineral density at the asymptomatic knees of patients with unilateral hip osteoarthritis. Arthritis Rheumatism 2011. [Google Scholar] [Crossref]
- N Shakoor, JA Block, S Shott, JP Case. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheumatism 2002. [Google Scholar] [Crossref]
- S. Clarke, C. Wakeley, J. Duddy, M. Sharif, I. Watt, K. Ellingham. Dual-energy X-ray absorptiometry applied to the assessment of tibial subchondral bone mineral density in osteoarthritis of the knee. Skeletal Radiol 2004. [Google Scholar] [Crossref]
- D Pan, L Tianye, Y Peng. Effects of proximal fibular osteotomy on stress changes in mild knee osteoarthritis with varus deformity: a finite element analysis. J Orthop Surg Res 2020. [Google Scholar]
- D N Utomo, F Mahyudin, A M Wijaya, L Widhiyanto. Proximal fibula osteotomy as an alternative to TKA and HTO in late-stage varus type of knee osteoarthritis. J Orthop 2018. [Google Scholar] [Crossref]
- Y L Dong, Y N Qian, Y M Li, L F Zhai, H Xu, C Y Cai. A comparative study of the curative effect of proximal fibular osteotomy and single condylar replacement for the treatment of knee osteoarthritis of different severity. Zhongguo Gu Shang 2020. [Google Scholar]
- M Ashraf, P P Purudappa, V Sakthivelnathan, S Sambandam, V Mounsamy. Proximal fibular osteotomy: Systematic review on its outcomes. World J Orthop 2020. [Google Scholar] [Crossref]
- S Shanmugasundaram, SBS Kambhampati, S Saseendar. Proximal fibular osteotomy in the treatment of medial osteoarthritis of the knee – A narrative review of literature. Knee Surg Related Res 2019. [Google Scholar] [Crossref]
- B Liu, W Chen, Q Zhang, X Yan, F Zhang, T Dong. Proximal fibular osteotomy to treat medial compartment knee osteoarthritis: Preoperational factors for short-term prognosis. PLoS One 2018. [Google Scholar]
