Introduction
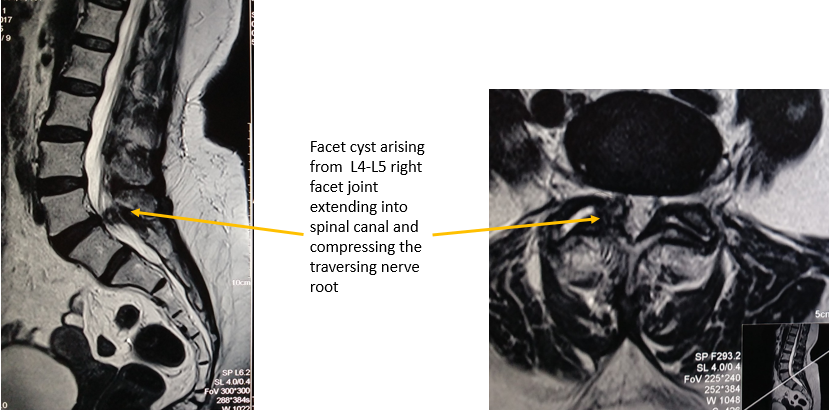
Lumbar intervertebral disc prolapse and sciatic pain has been in a focus since many years. Though Mixter and Barr in 1932 published it as only one cause of sciatic pain and gave surgical disc excision as treatment, sciatica still continues to perplex many physicians who proclaim a bulging disc as the cause of radicular symptoms, but find no obvious herniated fragment on surgical exploration. It occurs because physicians overlook other findings on a MRI scan which can also present clinically similar to sciatica. (Figure 1)
Spine surgery has advanced many folds in the past few decades but the complexity to arrive at the right diagnosis has not become simpler. Even in the presence of advanced radiological techniques like MRI (with or without contrast) and CT (with and without myelogram) the incidence of failed back surgeries is increasing. Through this article we try to dispel some uncertainties about disc herniation and study in detail its aetiology, treatments available, their indications and their clinical outcomes.
Figure 1
64 years male presenting with facet cyst at L4-L5 level along with L4-L5 disc bulge. Patient had right leg radiculopathy. Performing only discectomy in this case will lead to no relief in patient’s symptoms.
Etiology of disc herniation
Obesity (especially BMI > 30 2
Diabetes mellitus and hyperlipidaemia (affect microcirculation of the disc 3
Smokers (affect microcirculation of the disc and frequent coughing increase strain on the annulus 4
Driving for long hours, physically demanding work, manual labour and prolonged sitting (increased twisting, bending and vibration from machinery) 5
Genetic predisposition (positive family h/o disc herniation 6
Acute trauma 7
Mobility (lumbar spine is the most common site of disc herniation while thoracic spine is least involved) 8
Anatomy & biochemical structure of an intervertebral disc
Intervertebral disc (IVD) is the largest avascular, anural and alymphatic organ of our body. 9 A single intervertebral disc is composed of 3 components:
Two cartilaginous end plates on either side, adjoining the adjacent vertebrae
Nucleus pulposus: a gelatinous pulpy core
Annulus fibrosus: a tough fibrous layer which holds the gelatinous pulp in its place 10
These structure act synergistically to convert shock loads on the vertebral bodies to a smooth movement.
Biomechanics of loading forces on an intervertebral disc
Forces acting on a disc produced by loading can mainly be divided into three groups
Annulus is a highly resilient structure. It takes very high forces for nucleus to rupture an intact young annulus and herniate out of its periphery. 11 But since many patients give history of only a trivial trauma like lifting weight or an unbalanced fall, high energy trauma cannot be the sole factor for disc herniation.
Disc failure has been studied to occur through follow ways
Annulus integrity breaks from inside progressing to its outer border. This happens when the extracellular matrix becomes altered and weak in a degenerating disc.
Forces acting on annulus exceed its tensile strength and break its outer borders. The crack subsequently progresses inwards towards the nucleus with further movements and injuries.
Repetitive loads along with the degenerative cascade, over years lead to gradual breakdown of annular fibres. Posterolateral region is inheritably the weakest area in the annulus and henceforth becomes the most common site of nucleus herniation. It is important to note that for a nucleus should by well hydrated to herniate through the cracked annulus. Therefore disc herniation is more common in individuals in their 3rd and 4th decades of life.
Investigations
Of all the radiological investigations MRI plays the most important role as it helps delineate the soft tissue structures exceptionally well. (Figure 2)
High quality 3 Tesla MRI helps to:
Confirm the diagnosis of disc herniation and rule out other pathologies
Shows the size of the herniated disc
Shows the morphology of herniation: symmetric disc bulge, asymmetric disc bulge (not considered as disc herniation but can cause radicular symptoms), focal protrusion, broad based protrusion, extrusion, and sequestration.11
Shows the location of herniation: central, paracentral/ subarticular, foraminal, extraforaminal
Shows if the disc herniation is contained or non-contained
Shows migration of fragments: superior, inferior, axillary, intradural12, 13
Assess the extent of nerve root compromise14
Assess the health status of other discs
Assess the size of intervertebral neural foramina
Decide if the patient can be managed conservatively or will need decompression
Decide the surgical approach to the procedure
Electrophysiological tests
In cases where MRI does not correspond to clinical findings, electrophysiological testing (EMG & NCV) is a useful tool to investigate metabolic, central neurological and peripheral neurological causes for radiculopathy besides nerve root compression at disc level.
Blocks
In cases where MRI shows multiple level disc herniation, it can be difficult to identify the right pathological level. In such cases epidural, selective nerve root injections and intraarticular injections in the facets and SI joints can be used as diagnostic tools to locate the pathology.
Treatment
Non operative treatment
When the patient presents with sciatica for the first time in the outpatient department, in the absence of the following indications the patient can always be started on a non-operative trial
H/o significant trauma
C/o loss of bowel or bladder control
C/o saddle anaesthesia
C/o bilateral lower limb weakness
C/o rapidly progressing neurological deficit
The patient should be managed non-operatively with:
Reassurance
2. Short period of bed rest (2-3 days) especially in a semi-fowler position It helps by unloading the spine 11 (Figure 3)
Nonsteroidal anti-inflammatory drugs (NSAIDS
Muscle relaxants if required
Heat massage/ ice therapy
Analgesics (acetaminophen preferred Avoid nephrotoxic drugs
Anticonvulsants
Gabapentin and pregabalin have been found to have a beneficial role in neuropathic pain 15
Figure 3
Semi- Fowler positon: Patient lies relaxed with hips and knees flexed. This position can also be achieved in lateral decubitus by maintaining flexion at hips and knees.

The patient should be followed weekly and repeat physical and neurological examination should be performed at every visit. If there is adequate pain relief and no further neurologic deficit, the patient can be started on physiotherapy. This includes back stretching, back strengthening and back schools. The type of exercise depends on how long the patient has been disabled and on the grade of muscle atrophy. The patient should be advised modification of his/ her activities which includes to avoid prolonged sitting, forward bending and lifting heavy weights. Most of the patients recover in 4-6 weeks and are allowed to get back to their daily routine life with above mentioned precautions.16
If there is no improvement from the non-operative management at the end of 4-6 weeks or if there is a progressive neurological deficit or if there is cauda equina syndrome, the patient is advised urgent radiological investigations. Of all the radiological investigations MRI plays the most important role as it helps delineate the soft tissue structures exceptionally well.
Epidural and selective nerve root block (SNRB)
This procedure is a part of the non-operative management besides being a diagnostic aid. The block is a mixture of a local anaesthetic (0.25% bupivacaine or 0.5% lignocaine) and a corticosteroid (triamcinolone acetate or methylprednisolone) which is delivered at the target level (herniated disc) under fluoroscopic guidance to help relieve the acute radicular pain by its anesthetic and anti- inflammatory action. (Figure 4)
Indications for the SNRB include
Patient with herniated disc with a severe root compression not willing to undergo surgery
Disc morphology not correlating to the clinical symptoms : it helps confirm if the cause of the radicular pain is the same herniated disc or something else (Figure 5)
Predict the outcome: a patient getting relief from the SNRB will have a favourable outcome if treated surgically.
Atypical extremity pain 17
A single shot of epidural or SNRB provides short term relief of around 3 months. It is proven that a patient can delay his her surgery for a few years if they respond well to SNRB or epidural blocks. A patient can have a maximum of 4 injections in a year. Each injection must have a gap of 1-2 weeks in between. 18, 19
Operative Treatment
Indications
All the patients with acute disc herniation:
Who have failed a non-operative and epidural/ SNRB trial for 3 -4 months, do not have waddle signs or symptoms and are not involvement in workers compensation litigation. 20
Have cauda equina syndrome
Have progressive neurological deficit
Chemonucleolysis
Chymopapain is proteinase enzyme extracted from papaya fruit. It has high activity over nucleus pulposus. It breaks the proteoglycan chain and decreases the water holding capacity of the nucleus. Henceforth the nucleus shrinks and the compression is relieved. But it has poor action in extruded/ sequestered disc herniation (because they have lower proteoglycan and higher collagen content), calcified disc herniation, bony canal/ foramen stenosisand instability.
It can pose some serious complications (hypersensitivity, anaphylaxis, subarachnoid haemorrhage and transverse myelitis). Therefore it is not a very popular procedure.
Conventional open discectomy
The technique
The patient is given general endotracheal anaesthesia and placed in a prone position in a Jackson (OSI) table or Andrews spine frame. The target disc space and inter spinous space is identified by palpating the landmarks (iliac crest is at L4-L5 inter spinous space). Same is confirmed on fluoroscopy. A midline incision about 3-5 cm is placed at the target level from rostral to the caudal spinous process. The subcutaneous tissue is dissected and the deep dorsolumbar fascia is incised. Sub periosteal dissection of the para spinal muscles is performed using a bovie from the tip spinous process to its base (the spino-laminar junction). Now using blunt dissection the muscles are retracted laterally with a Cobbs retractor without violating the facet joint capsule. The target inter laminar space is exposed and is confirmed on fluoroscopy before proceeding further. A Taylor retractor is placed lateral to the faect joint. Using curettes, Kerrison rongeurs, nerve and dura retractors the overlying tissue, ligamentum flavum and lamina bone is removed. Medial facetectomy without compromising the stability of the facet joint (not more than 1/3rd of the facet should be resected) is performed. Dura and the traversing roots are visualised. The nerve root is retracted medially and the disc is identified. The annulus is cut and the target fragment is extirpated. Adequate decompression is confirmed if the angled hooks can be passed above and below the root in the neural foramina, nerve root is mobile and there are no visible fragment inside the canal. Hemostasis is achieved and the wound is closed in layers.
The extent of removal of bone from lamina of 3 types:
For a large central disc herniation, cauda equine syndrome and intra-dural migrated disc laminectomy (entire lamina from medial border of one facet to medial border of opposite facet) is performed.
For superiorly or inferiorly migrated disc and lateral recess stenosis hemi laminectomy (from medial border of one facet to the base of spinous process) is adequate.
For rest all cases minimal bone resection (fenestration/ laminotomy) is enough to expose the root and the lateral border of dura. 23
Micro discectomy
Microsurgery using magnification from microscopes were innovations that limited these surgical insults with equally effective decompression. 24 (Figure 6) Specialised burr drills give freedom to remove bone effectively with minimal hand movement in the limited space. (Figure 7) The surgical technique is same as the standard open procedure. The differences are
Smaller incision (2-3cm
Minimal damage to soft tissue
Microscope magnifies the structures in view allowing
Minimises risk of postoperative instability and back pain as the bone and soft tissue are preserved to maximum.
Minimal blood loss
Reduced postoperative hospital stay
Faster post-operative recovery
Endoscopic discectomy
Endoscopic discectomy is a step further to reduce the skin incision length and minimize soft tissue injury. This method was first introduced by Kambin and Hijikata. 25, 21 Currently there are four techniques to do it
Micro endoscopic discectomy using tubular retractors
This technique was given by Foley and Smith in 1997.26 Tubular retractors split the muscles and radially dilate the muscle fibers. They trick is to not cut through the muscle fibers. This reduces the muscle injury. Specialized serial dilating tubes and retractors are used which have attached light sources. This allows for smaller incisions with excellent view of the underlying structures. (Figure 8)
The technique
With patient in prone position, an AP shot is taken on the C-arm machine and ipsilateral inferior pedicle of the target level is identified and marked. Lateral view is taken to confirm the target level. For a left sided L4-L5 disc, left side L5 pedicle is marked. A 1-2 cm incision is made in the skin and the underlying dorso-lumbar fascia. Specialized serial dilators are then progressed with a rotatory motion that allows separation and serial dilation of muscle fibers.
The dilators are docked onto the inferior L4 facet and confirmed radiologically. After a satisfactory position is achieved specialized expandable retractors are inserted and serial dilators are removed. The retractor system is fixed to a flexible arm rigidly fixed to the operating table. The light source is attached.
The rest of the procedure is same as microscopic discectomy using specialized bayoneted instruments and burr drill.
The Destandau technique
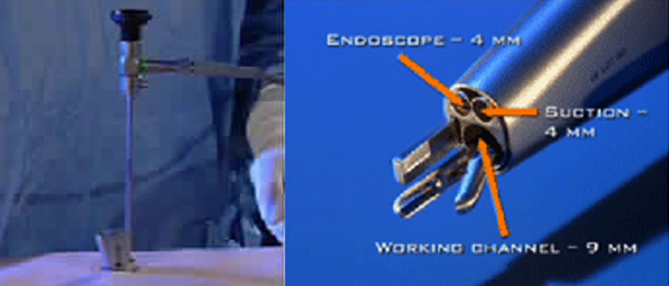
This technique was described by Jean Destandau in 1999. He developed a specialized endoscopic spine system (Endospine) and approached the spine via the posterior inter laminar approach. 26, 27
This specialized endospine system consists of two detachable tubes: outer tube and inner tube along with an endoscope. The inner tube has 4 built in channels, each for endoscope, suction, working instruments and nerve root retraction.(Figure 9)
The technique
Under endotracheal anaesthesia the patient is placed in knee chest position.
The target inter laminar space is marked under fluoroscopy. A para median 1-1.5 cm long incision, about 1 cm from midline towards the affected side is made. Skin and underlying dorso- lumbar fascia is incised and the para spinal muscles are lifted subperiosteally off the spinous process and lamina. The outer tube is placed and docked at the target inter laminar space. Then the inner tube is placed. The endoscope is passed through its channel. The rest of the decompression is same as microscopic discectomy using its specialised instruments.
Full endoscopic inter laminar discectomy
In this technique endoscopes has angled lenses. Angled endoscopic lenses allow for greater field of vision. These endoscopes have built in channels for working instruments and light source. These endoscopes are passed through a working cannula and docked at the target inter laminar.
The technique
With patient in endotracheal anaesthesia and in prone position, the target inter laminar space is marked on AP and lateral fluoroscopy view. An 8-10 mm incision is made close to the midline. Skin and dorso-lumbar fascia is incised. Blunt tipped dilators are inserted and docket over the target inter laminar space. After confirmation a bevelled working cannula is introduced and the dilator is removed. The position is again confirmed on fluoroscopy. After confirming the level, the endoscope is introduced. Using the specialised long instruments through the channels in endoscopes, the decompression is performed similar to as in microscopic discectomy.
Full endoscopic trans foraminal discectomy
Also called percutaneous trans foraminal endoscopic discectomy (PTED). The procedure can be performed in endotracheal and local anesthesia as per the comfort of the physician. (Figure 10)
Here the disc is approached posterolaterally through the intervertebral foramen. This technique was given by Kambin in1992.28 He described a safe pathway for endoscope and its instruments called as ‘Kambin’s triangle’. It is a zone bounded with the following boundaries (Figure 11)
Anterolateral: exiting nerve root
Posteromedial: superior facet of caudal vertebra
Inferior: superior end plate of caudal vertebra
Accessing the disc through this zone involves minimal risk to neural structures. The equipment involves angled endoscope with an irrigation channel and working channel, long spinal needles, bunt guidewires, dilators, beveled cannula, specialized long handled discectomy instruments and a radiofrequency probe.
The technique
The procedure can be performed in both local and endotracheal anesthesia as per the comfort of the physician. The most crucial step of this procedure is marking the right entry point. With the patient in prone position the abdomen is made free of pressure. Next, under fluoroscopic guidance, two line are marked on the skin using the AP view of the target disc space.
With pedicle equidistant from spinous processes midline of lumbar spine joining the spinous processes. (line A)
Midline of target intervertebral disc space with line parallel to the end plates of adjoining vertebra. (line B)
Additional lines are drawn on the skin using the lateral fluoroscopic view of the target disc space
Midline of target intervertebral disc space with line parallel to the end plates of adjoining vertebra (line C)
Line joining the posterior borders of the facets of lumbar spine (line D
Iliac crest border is marked using finger palpation (line E) The entry point lies in the area enclosed between lines B, C and D
The needle is inserted and directed towards the target disc space at an angle of 20 degrees to the floor. The needle is advanced under fluoroscopic guidance. Keeping the kambin’s triangle boundaries in mind, the needle is proceeded to the medial border of the pedicle on AP view and posterior vertebral line in of target disc space on lateral fluoroscopic view.
Now the annulus is pierced and disc is entered. Now discography is performed and indigo carmine dye is injected through the needle into the disc. The dye stains the nucleus blue. Now the needle is replaced with guidewire and over it dilator, beveled cannula and finally the endoscope are progressed. Next step is to access the herniated fragment. Using specialized shavers, drills, curettes and other instruments discectomy is performed.
Electro thermal annuloplasty
Procedure was initially introduced to relieve the patients of the pain in sciatica. It involves introducing an electro thermal coil into the outer annulus via posterolateral approach. The heat cauterizes the nerve endings and contracts the collagen fibers.
Coablation Nucleoplasty
Indicated only for contained herniation, using a posterolateral approach a needle is inserted into the target nucleus pulposus and radiofrequency waves are delivered to dissolve the soft nucleus and decompress the nerve.
Percutaneous Laser disc decompression
Using posterolateral approach laser energy is used through a needle to vaporize the water in the nucleus and shrink the disc fragment. The results have been limited and many cases required discectomy at a later stage. 28
Ozone nucleolysis
Indicated for contained disc herniation ozone is delivered to the target nucleus through the ‘kambin’s triangle’ zone via the transforaminal route. Ozone reacts with nucleus water and generates peroxide and hydroxyl ions. These ions break the nucleus and reduce its size.
Gelified ethanol, infliximab (anti TNF x) and collagenase
Ethanol mixed with ethyl-cellulose and radiopaque material for treating lumbar disc herniation has been presented in literature. 29 Similarly infliximab and collagenase have been tried but the long term results of these methods have been equivocal. 30, 31
Special situations
Migrated disc herniation
Disc migration has been classified by Lee et al into
Zone 1: far up: from inferior margin of superior pedicle to 3mm below
Zone 2: near up : within 3mm of inferior end plate of rostral vertebral body
Zone 3: near down: from superior end plate of caudal vertebral body to centre of inferior pedicle
Zone 4: far down: from centre of inferior pedicle to inferior border of inferior pedicle. 32
Another classification system has been given Ahn et al. They coined the terms low grade up and down for zone 2 and zone 3 respectively, high grade up and down for zone 1 and zone 4 respectively. They introduced one more grade:
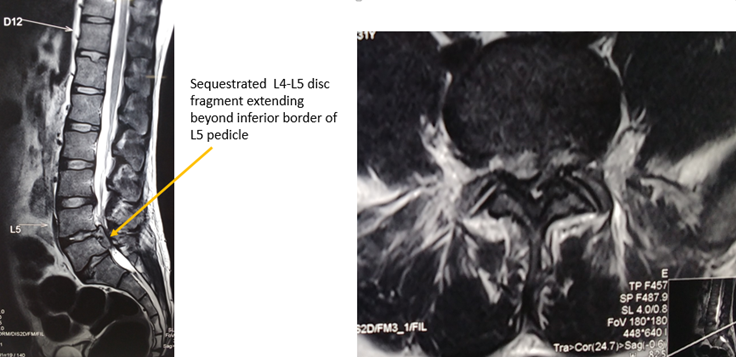
Very high grade: when the disc fragment migrated beyond the inferior margin of the pedicle on either rostral or caudal side. 33 (Figure 12, Figure 13)
Open/ microscopic technique
When using open or microscopic techniques, for very high grade migration it is recommended to approach from the superior border of the lamina of the pedicle where the fragment is residing.
For low and high grade migrations resecting extra bone using open or microscopic approaches is required. Care should be taken to avoid too much bone removal leading to instability.
Interlaminar
Similar to microscopic techniques. Due to freedom of mobility the endoscopes can be angled and flexible instruments can be used to retrieve the migrated fragment. If any difficulty is faced, converting the procedure to microscopic technique is the prudent answer.
Endoscopic techniques
Transforaminal approach from ipsilateral side is very good procedure for such herniation.
Interlaminar approach can use flexible instruments from the contralateral side. Requires very high expertise for the same.
Extra foraminal/ far lateral disc herniation (Figure 14)
Endoscopic techniques
Transforminal approach is best suited for such case scenarios while interlaminar approach should be avoided.
Recurrent disc herniation (Figure 15)
A patient presenting with a recurrence of similar signs and symptoms after a symptom free interval post primary discectomy surgery should be evaluated with contrast MRI. Epidural fibrosis, arachnoiditis and postoperative granulation tissue should be excluded. After the recurrent fragment has been identified on the MRI scan the patient can be taken up for revision micro discectomy. The fragment appears as hypo intense on T2WI.
Figure 15
70 year old male presented with recurrent disc herniation. The contrast MRI showed low signal core with hyper-intense margins due to peripheral neovascularisation of sequestrated disc fragment. (Contrast MRI is the modality of choice to diagnose recurrent disc herniation.

The dura is thinned out due to recurrent herniation and it is easily possible to have a dural tear. These surgeries are best performed using microscopes and wide decompression. 34
Cauda equina syndrome (Figure 16)
Emergency surgical decompression within 48 hours of onset of symptoms is advised. 35, 36 Surgery requires wide decompression (laminectomy + discectomy) using either open or microscopic approach. Endoscopic/ mini open approaches are contraindicated. 37, 38 Postoperative physiotherapy including pelvic floor exercises and multidisciplinary approach plays an important role in the recovery and rehabilitation of the patient. 39
Fusion
We advocate fusion only if preoperative or postoperative instability is suspected. Discectomy alone produces best results in absence of instability. 40, 41
Clinical outcomes
Non operative management vs Surgery
Surgical excision of the disc herniation is as obvious as removing a thorn stuck in the foot. Long term results of over 39000 patients were analysed and showed success rate of 78.9% over an average period of 6 years. This study gave good/excellent results for open discectomy in 78.3% patients, for microscopic discectomy in 84.3% patients and for endoscopic discectomy in 79.5% patients. 42 SPORT trial (RCT study) followed patients for 8 years and compared the results of operated vs non-operatively managed patients using SF- 36 and ODI scores. The results showed clinically significant improvements in the operated patients and there was no degradation in their symptoms over the next 8 year period. 43 Maine lumbar spine study reported greater improvement at one year in surgically treated patients. 44 Spetzger showed 93% success rate following surgery. A 5 year study by Rish L found out of the total patients who were treated with conservative surgery, 41% patients required surgery. In carefully selected patients they found the success rate of surgery was more than 90%. 45
Open vs microscopic discectomy
Well performed decompression in carefully selected patients with proper indication for surgery had similar clinical outcomes in terms of pain relief, neurological recovery, complications: dural tear, root injury, reoperation rate and patient satisfaction. Micro discectomy had longer learning curve and longer operative time but was superior in terms of lesser blood loss, lesser tissue damage, lesser post-operative back pain, early mobilisation, shorter hospital stay and early patient recovery. 46, 47, 48, 49
Microscopic vs tubular vs fully endoscopic inter laminar discectomy
Outcome measure were ODI, VAS back and leg pain, Modified McNab criterion, and serum CPK levels pre op and post op. As per modified McNab criterion all three groups showed good to excellent results in > 90% patients. VAS and ODI improved significantly in all three groups and their results were similar. But endoscopic and tubular techniques had lesser post op back pain compared to the micro discectomy group. Post-operative MRI showed that dura expansion in all three groups was similar. The blood loss was least in endoscopic and maximum in microscopic group. The endoscopic group had shortest hospital stay period. Endoscopic group had least rise in serum CPK levels post op. The disadvantage was longer operative time and longer learning curve for tubular and endoscopic techniques. 50 Similar results have been supported in many other studies. 51
Many studies support smaller incision leads to minimal soft tissue dissection and minimal blood loss leading to less muscle injury, less iatrogenic denervation and less back pain. 52, 53, 54, 55, 56, 57, 58
Conclusion
It is important to note that discectomy performed in patients with non-contained disc herniation (sequestration/ trans ligamentous extrusion) show best relief from surgery followed by contained but ruptured disc herniation (sub ligamentous extrusion) and contained non-ruptured disc herniation (focal protrusion). The poorest results are for patients who are operated for broad based disc protrusion/ bulge which are not true herniation though they can compress upon a nearby nerve root in a pre-existing foraminal/ lateral recess stenosis. In the former case scenarios at the time of surgery if a window is cut into the annulus the nucleus will extrude spontaneously and the pathological fragment will be removed. But same does not happen for broad based protrusions or disc bulges as the pathological fragment cannot be located and the exploration turn out to be negative. 59 This is how the term concealed fragment creeped into the literature. 60
The takeaway message is to study the MRI films, both the axial and sagittal images carefully. Focussing only on a disc with expanded borders beyond its normal contour can make the physician miss the real cause and lead to a futile trip of the patient to the operation theatre. In carefully identified patients, surgery has excellent results. The surgical technique should depend on the expertise of the treating physician as the clinical outcomes in terms of pain relief and neurological recovery are equally good in all well performed techniques.
Minimally invasive techniques show faster and better post-operative recovery but only in hands of well-trained physicians.